This Physical Examination review is written specifically to help you understand the logic behind the NBCE Part IV Physical Examination section and the Tests/Examinations commonly asked by NBCE. By now, we believe that each individual taking the Part IV examination already knows how to perform a thorough physical examination. Please refer to your notes, books, or other study guides if you are unsure about how to perform a certain examination. With that in mind, this section will place an emphasis on important topics, strategies, and techniques needed to excel on the physical examination section of the chiropractic national board part IV. It should be noted that you will not be asked to perform a full physical examination during the NBCE Part IV examination. You will only be asked to perform few "specific examinations" such as Auscultation of the heart, Tactile Fremitus, Auscultation of the lungs etc. In other words, NBCE will not ask you to perform a full examination of the heart, lungs, abdomen or other areas of the body. They will only ask you to perform a "specific examination" for a certain organ (heart, lung, liver, kidney) or region of the body as mentioned above.
|
Introduction and Overview
The physical examination section constitutes a minor portion/percentage (5-10%) of your total score compared to other sections, and there will be only one pre-station and one post-station for this section. Although it constitutes a small portion of your total score, we highly recommend that you spend quality time reviewing and studying for this section. Having a good background in physical diagnosis will strengthen your ability to come up with appropriate differentials during the course of your examinations and history taking regardless of the station you are in (ortho/neuro, physical diagnosis or case history). Simply review and practice what is provided in this section and CNBA will provide you with the most important topics that should be covered in the physical examination section. The purpose of this review is to prepare you in such a manner that you understand what is required of you and how the examination should be taken. This section will allow you to understand what is required of you during the examination and will provide you with important and valuable information that will assist you throughout other stations.
For the physical examination station, the observing doctor of chiropractic will grade you based on your ability to perform the examinations correctly, your ability to properly and correctly evaluate the patient by asking appropriate questions, and your ability to properly interact with the patient. It is highly recommended that you show incredible amount of consideration for the patients as you perform the examinations. Again, it should be noted that you will NOT be asked to perform a detailed/full physical examination. You will only be asked to perform specific and random examinations for each region of the body such as auscultation of the valves of the heart, tactile fremitus, percussion of the chest, or deep and superficial palpation of the abdomen. Therefore, you will not be asked to perform a full examination of the heart, abdomen, lungs or other areas of the body. CNBA has provided in this section the examinations that you would need to know for the NBCE Part IV physical examination section.
The Examination:
You will not be required or allowed to bring your own tools to perform the examination(s). As you enter the pre-station room, there will be a few examination tools displayed for you to use such as a reflex hammer, stethoscope, tuning forks, pinwheel (NBCE may also use toothpicks along with cotton balls instead of a pinwheel for dermatome testing), etc. For example: NBCE may display a 128 Hz tuning fork along with a 512Hz tuning fork, and ask you to perform a vibratory test. In this situation you would have to choose the correct tuning fork for the examination, which would be the 128Hz for vibratory test. If you chose the incorrect tuning fork, you will lose major points for that section. If they have a stethoscope and the examination does not ask you to auscultate any part of the body, then you should NOT. Only perform what is asked of you, and use good judgment in choosing the correct tool for the examination.
You are also allowed to interact with the patient during the course of the examination and ask questions related to their problem(s), however, you may not speak with the observing doctor at any time for he or she will not respond or assist you. For example, if a patient presents with chest pain, you are allowed to and should interact and ask the patient questions to determine whether the patient has a condition related to the heart, lung(s), a broken rib(s), costochondritis, esophagitis, hiatal hernia (GERD) and all possible conditions that may produce chest pain. Most students make the mistake by assuming that by simply perfoming the examinations required of them, that they will automatically gather enough information needed to thoroughly answer the questions in the post-stations. This assumption is False. You must ask specific quesions throughout the examination to rule in and rule out certain conditions. We highly recommend and advise that every student should perform a mini 30 second history prior to starting the examination. This will allow you to develop a better understanding of the patient's condition, and will therefore give you an opportunity to come up with a few important differential diagnoses. The student should also expand on each examination finding and continue to ask the patient detailed questions during the course of the examination to rule in or rule out certain conditions. Remember, you will also be graded on whether you are capable of obtaining valuable data from the patient and whether you are capable of asking the patient important and necessary questions that will lead you toward the final diagnosis. This section will cover the most important questions that should be addressed before, during, and after you perform the examinations. We have also included notes, and important strategic concepts to help you with the physical diagnosis examination section.
Back to Top of Page
|
Tips and Scenarios:
Ask questions before, during, and after you examine the patient. Silently examining the patient could cost you points and prevent you from obtaining valuable information. The patients have been instructed by NBCE to provide information regarding their condition only if appropriate types of questions are asked. For that matter, you must not only perform the listed examinations or tests correctly, but you must also ask specific questions and look for associated symptoms, which will play a significant role in your ability to come up with important differentials and finally a concrete diagnosis. Lastly, you should always indicate out loud what examination you will be performing, and give the patient specific instructions prior to performing an examination. Feel confident as you are performing the examinations and don't stress out.
Case 1:
This physical examination case will help you develop a better understanding of how the examinations may be presented and what is expected of you. Below is an example of how NBCE may display the instructions:
STATION 1
INSTRUCTIONS TO CANDIDATE
PATIENT DATA
Name: Joanne Richardson
Age: 55
Occupation: Retired school teacher
Presents with Chest pain.
PERFORM A FOCUSED PHYSICAL EXAMINATION
1) Auscultation of the lungs
2) Percussion of the heart
3) Palpation of the pulses of the upper extremities
4) Sternal Compression Test
5) Schepelmann's Test
NOTE: At the next station (2) you will be required to answer questions related to this patient's condition
Please have your (2) identification labels ready |
It should be noted again that the patients are simulated and are acting out conditions. Therefore, these patients will most of the time either indicate that they currently have some kind of pain, or state that they have or have had certain types of signs or symptoms in the past associated with their current condition (so make sure you also address the patient's past during the examinations and not simply the present).
Let us begin with the first examination listed above which would be Auscultation of the lungs. As you auscultate her lungs, you should assume that there is realistically nothing wrong with the lungs, and that you will not expect to hear anything abnormal. In other words, don't try too hard to pick up an abnormal sound because there will not be any (the patient is normal in reality). In some cases, however, if the patient is simulating a lung condition, it would be possible for her to act out symptoms associated with her condition such as coughing, wheezing or indicating that she has difficulty and pain with breathing. She may even be holding an inhaler to show that she may have asthma, or COPD, but she will not be able to act out stridor, crackles or any other strange or abnormal lung sounds. Prior to performing the examination, explain to her what you are attempting to do and have her inform you if she experiences pain or discomfort during the examination. If she begins to complain during any of the examinations listed above such as auscultation of the lungs for example, use correct judgment to figure out if her complaint might be lung related (pleurisy, pulmonary embolism, lung cancer etc.) or a possible musculoskeletal condition such as costochondritis or a rib fracture, which could also cause pain with deep inspiration/expiration. There would indeed have to be some type of an injury or trauma if you are suspecting a rib fracture. If she states that she did not experience any pain or discomfort and no unusual sounds were heard during the examination (auscultation of the lungs) then simply state to the observing doctor that your findings were normal and move on to the next examination (at this point you were simply being evaluated on whether you were able to correctly perform the examination). Now, NBCE has in the past played audio recordings of normal and abnormal lung sounds, heart sounds etc. and has asked students to indicate whether those sounds are normal or abnormal; but NBCE has not asked students to name or identify the exact sound being played. If an audio recording is played, your responsibility will be to simply address whether the sound is “normal” or “abnormal”. For more information regarding lung sounds you may visit the following websites provided below and download or play normal and abnormal lung sounds: CNBA is in no way affiliated with these websites.
1) http://www.stethographics.com/main/physiology_ls_introduction.html
2) http://faculty.etsu.edu/arnall/www/public_html/heartlung/breathsounds/contents.html
As a general rule, if NBCE asks you to perform an examination in a certain region of the body where the patient will not be able to act out the condition such as abnormal lung sounds, palpitations, murmurs, ejection clicks, mitral stenosis, abnormal bowel sounds, bruits etc., or symptoms associated with these conditions, then assume that there is nothing wrong with that particular body part or region. The above statement holds true unless the patient states that he or she is either experiencing pain or discomfort during that specific examination that you are performing or further history taking proves that the patient has that particular condition associated with the body part or region in question. Here's why this assumption holds true. NBCE will not bring patients that have serious medical conditions and allow students to examine them for the sake of evaluating their competency. If NBCE asks you to examine (this may be auscultation or palpation) the patient's abdominal aorta, simply perform the examination and indicate that your findings were normal (the actual patient will not have an abnormal sound (bruits) or abnormal pulsations associated with an abdominal aortic aneurysm). Now, the patient may state that he or she experienced pain with auscultation or palpation of the abdominal aorta (this would indicate that although an abnormal sound or pulse was not heard or felt, the patient does indeed have an underlying problem, and it would be your responsibility to determine the cause of pain by asking the correct types of questions). In other words, you would need to ask the patient if he or she is experiencing any other signs or symptoms typical of an abdominal aortic aneurysm or other underlying abdominal conditions. With these examinations, NBCE's main concern is to see if you're able to perform these examinations correctly and how you're interacting with the patient during the examination. If your history taking skills are excellent, and you manage to obtain valuable information simply by asking proper questions in addition to performing the examinations, you will have a much higher chance of properly diagnosing the patient as opposed to basing your diagnosis from your objective findings/examinations alone.
Always instruct the patient to directly indicate if he or she is experiencing pain or any type of discomfort during these examinations ( Most of the time these patients will show signs of apprehension or will make facial gestures which indicate pain or discomfort, which you might miss if you are not careful or observant. Having the patient indicate that he or she is experiencing pain during an examination will allow you to take under consideration which examinations produced positive findings.) If you palpate the abdominal aorta and the patient indicates he or she is experiencing pain, then assume that there might be something wrong with the abdominal aorta and begin asking questions related to this region and condition to rule in or rule out an AAA first, even if your physical examination findings during the palpation of the abdominal aorta were normal (This means: You did not feel any unusual pulsations during palpation of the Abdominal Aorta but the patient complained of pain during this particular examination, which could suggest a possible AAA). If the patient does indicate that he or she experienced pain, do not assume that your findings were abnormal and that the patient automatically has AAA because you are not sure at this point. If the patient directly states “I'm having pain” or says “Ouch” as you are performing palpation of the abdominal aorta, then simply ask the patient additional questions such as the ones listed in Table 29 to prove or disprove AAA.
Now, as you perform the second examination displayed above, which was percussion of the heart, the patient can indicate here that she feels pain during percussion. In reality however, the examination is performed and the doctor tries to observe expanded areas of dullness which could possibly suggest cardiomegaly or pericardial effusion. Since the patient is acting out a condition in reality, assume that she does NOT have an enlarged heart or pericardial effusion, or any underlying heart condition that may be picked up by such an examination. The patient however, may indicate that she is experiencing pain during percussion, which may suggest cardiomegaly, pericardial effusion or even a musculoskeletal condition such as a rib fracture or an injured muscle. With all situations and conditions, you must ask specific questions to prove or disprove a condition in question (even if the examination findings are postive or negative). If you are suspecting a rib fracture, ask about possible trauma to the chest or body. If the patient denies any injury or trauma to the chest or the body, then you could rule out a rib fracture and so forth. Remember to take the patient's history and age into consideration. If the patient does NOT indicate that she is experiencing pain or any other symptoms during percussion, then simply indicate that your findings were normal and move on to the next examination. If the patient states that pain was produced with percussion of the heart, then you must readily have a list of questions in the back of your mind, which you will need to ask in order to determine the true cause of the pain. Such questions should consist of the following:
- Any history of HTN?
- Do you smoke, and if so how much? (make sure you have the patient indicate exactly what he or she smokes).
- If you do not smoke now, have you ever smoked in the past and how much did you smoke?
- Any recent history of trauma to the chest area or the body?
- Have you experienced these symptoms in the past?
- When did it start, how it started, and how long does it last when it starts?
- What were you doing when it started?
- Is it caused by activities?
- Is it stress related?
- Any shortness of breath?
- Is the pain deep or superficial?
- Any family history of HTN or Heart disease?
- Is the pain localized? If not, does it radiate and where to?
- Is the pain gradually getting worse or better?
- Any family history of lung cancer or lung disease?
- Any recent fever or unintentional weight loss?
|
At this point, these questions above will help you gather sufficient amount of information from the patient, which will assist you throughout the other examinations and allow you to fully answer the questions in the post-stations. In addition, you will come up with more questions as you begin performing the examinations and based on the patient's reaction to these examinations. If the patient answers yes to any of the questions provided above, then you must assume that it is important enough to elaborate on. If the patient indicates that she is a smoker, has Hypertension and her father died of a heart attack, then it is an indication that she might possibly have a heart related problem/condition (also look at blood results in the post station to confirm). To be safe, you must also ask more question(s) to rule out a possible lung related condition(s), because smokers tend to have Hypertension as well as lung problems. The following are a few of the important questions that should be addressed to rule out a possible lung related problem:
- Any history of coughing? (Is it productive or dry, and if so what color?)
- Any history of unintentional weight loss?
- Any history of CA or family history of lung CA?
- Any history of recent fever, and if so high grade or low grade?
- Any history of shortness of breath, difficulty breathing, or pain with breathing?
|
If the patient answers "NO" to any of these questions, then you can assume that this patient most likely does not have a lung condition and focus more on the heart.
It should be noted: If you are performing an examination that is meant to address the heart for example (e.g. auscultation of the heart) and the patient admits to having pain as well as symptoms associated with a heart condition during that particular examination, then it is a high indication that the patient is indeed simulating a condition related to the heart. Same thing applies to all other organs or regions of the body. On the other hand, if NBCE for example asks you to palpate the abdominal aorta (usually done to determine a possible AAA) and the patient presents with pain during that examination but doesn't have symptoms associated with an AAA, then Abdominal Aortic Aneurysm can not be concluded simply because the patient presented pain during palpation of the abdominal aorta. Therefore, further questions should always be asked along with a positive examination finding to address the true etiology of the patient's pain or problem.
The third examination listed above was palpation of the pulses of upper extremities. Palpation of the pulses of upper extremities is also going to be normal because the patient cannot intentionally alter the rhythm, amplitude, and contour of her pulse. In this case, NBCE wants to assess whether you know how to perform the examination correctly. In addition, you should ask her if she has ever had coldness of the hands or feet, or abnormal discoloration of the extremities. This will allow you to determine if the patient might have a possible vascular condition as well.
The fourth examination listed above was Sternal Compression. The Sternal Compression test is used to rule out a fracture and is mostly used in traumatic related injuries. If the patient does not complain of any pain during the examination and has had no history of trauma, then the test will most likely be negative. On the other hand, if a patient does complain of pain, always ask the patient to point to the exact location of pain, have them describe the quality and depth of pain, and ask if the pain radiates or is localized in nature.
Lastly, Schepelmann's Test will help you determine if the patient's condition is musculoskeletal in nature or visceral (Intercostal neuritis vs. dry pleurisy) .
The intention of this example was to show a few possibilities associated with a patient's complaint, what to expect as you perform a certain examination, how much limitation a patient may have while acting out or "simulating" a condition, and a general overview of how the physical examination section may be presented. In conclusion, by simply performing the examinations and not asking necessary questions to rule in or rule out certain conditions, you will not obtain enough information to thoroughly and correctly answer the questions in the post-stations. Back to Top of Page
Important Considerations
If NBCE asks you to perform an examination such as auscultation of the heart or the lungs or the abdominal arteries, then we can assure you that these patients will not have an apparent or actual heart, lung or vascular condition, for it would not be rational to bring in a patient that is having a true heart attack, or a patient with pneumonia or a patient with a carotid or abdominal bruits. If NBCE asks you to auscultate the abdominal aorta, then bear in mind that this patient will NOT have bruit. Whether or not this patient may have a problem related to the Abdominal Aorta will be mostly based on the types of symptoms he or she is presenting with rather than the objective findings from the physical examination.
Another good example would be percussion of the heart. This examination is primarily used to determine a possible enlarged heart or pericardial effusion. It is once again worth noting that these patients will not have an enlarged heart, so therefore, don't assume that the patient does have an enlarged heart as you are performing this examination. NBCE simply wants to see if you are capable of performing the examination correctly. With these examinations, you should always ask if the patient is experiencing pain or discomfort and have them share with you the symptoms that they experience or have experienced in the past while performing the examination. Same concept applies if you are asked to perform an ophthalmoscopic examination of the eye. The patient CAN NOT fake and will not have an apparent glaucoma, papilledema or retinal hemorrhage upon examination. If you are asked to perform such examinations, perform the examinations correctly and accept that the findings are normal unless further history taking and certain symptoms expressed by the patient proves or disproves the presence of the condition.
In the post-stations, you will also be given additional information regarding the patients such as:
1. Additional History
2. Blood results
3. X-rays or other diagnostic images.
Back to Top of Page
NOTES
Inspection
1. Before you begin examining and questioning the patient, simply observe and inspect the patient for any abnormalities or clues that may be apparent. Always bring the clues listed below to the patient's attention if you notice them ( The observing doctor grading you wants to see the degree of your awareness ). If you do NOT mention or bring to the patient's attention that you see these clues, then it would be assumed by the observing doctor that you did NOT see them and you will lose points in that section of the examination.
Common possible clues to look for during the examination and their indications:
a. Wearing a hat, bandana or a scarf
- Patient might be hiding a scar or a mass/lump, is having major hair loss (alopecia), allergic to the sun, is prone to skin cancer, recovering from chemotherapy (bald) etc.
b. Wearing sunglasses
- Patient might be covering up a scar, had been in a recent fight/trauma, has photophobia (or other light sensitivities due to certain medications), had recent eye surgery, for reduction of headaches and eye-strain etc.
c. Wearing a brace
- Depending on the location, a brace is usually worn due to some kind of trauma/injury, pain, instability, post surgery, carpal tunnel, dislocation, overuse etc.
d. Sitting or standing in an awkward position
- Most musculoskeletal conditions are triggered or relieved with certain positions, and a patient may be avoiding a certain type of pain by simply standing in a certain position. Be aware of these signs (e.g. Minor's Sign, Amoss Sign, Tripod Sign in the course of the examination etc.) Ask the patient why they are sitting or standing in such a position. The patient will most likely indicate that this is the only position that gives him or her relief.
e. Holding an object in the hand (such as a cigarette pack, an inhaler or a picture of a loved one etc.)
- Always ask questions regarding the objects a patient is holding. (NBCE wants to see if you are able to observe these objects). A cigarette could indicate that the patient is a heavy smoker, has an underlying lung condition or needs help to quit. A picture of someone could indicate that a loved one has died and the patient is in severe depression. An inhaler could indicate that the patient has asthma or a lung related problem ( COPD ).
|
In general, if you see an object in the patient's hand or by the patient or in the examination room, feel free to ask the patient about the object (even if it's something the patient is wearing such as a hat, sunglasses, braces, bandanas etc). If the object is of no significance, the patient will tell you once you ask. If you disregard the object, the patient will never give you a clue or a direct answer, and you might not be able to fully answer the questions in the post station because you will not have the necessary information required to do so.
Hint: Here's how you should approach the following situation. First of all, Do NOT state to the observing doctor “I see the patient is wearing a brace” or “I see the patient is holding an inhaler”.
This is how it should be performed: As you approach the patient, state “I notice you are wearing a brace tell me what's going on and why you're wearing it?” or “I notice you're holding an inhaler tell me what's going on, is anything bothering you” or “I see you're wearing a jacket on a hot day is there anything wrong?” The patient will then begin to elaborate (if anything is wrong) as soon as you bring it to their attention. At this point, you have shown the observing doctor that you are aware and have recognized these clues. The patient will then begin to elaborate and this will open up more questions for you during the examination, and will give you a better understanding of the patient's overall condition.
Back to Top of Page
Other Considerations
Remember NOT to immediately perform the examinations as you enter the room without asking the patient a few questions regarding their chief complaint and present illness. For example, you may approach the patient in the following manner, “Hello Mr. Johnson, My name is ___________ and I am going to be performing your examination today. Before I begin to evaluate you and perform some examinations can you please tell me about your complaint and what brought you here today? This process gives you an idea of what to expect and how you will approach the patient during the examination. If a patient states I fell on my shoulder, then it would be highly advisable that you are very gentle with the patient. You could then state, “I'm sorry to hear that Mr. Johnson ( you're showing concern ), before I begin to evaluate you I will be explaining to you what I'm going to do and if at any time you feel uncomfortable or I cause more pain during the examination I want you to let me know ok? This is a critical step because NBCE also grades you on patient interaction and consideration. If you enter the room and immediately start your examinations without asking the patient questions or permission from the patient, it clearly shows lack of clinical skills necessary to handle actual patients, and you will lose points in that section. As a general rule, for every station, not including the technique stations, you must initially (for about 30 seconds) ask a few questions regarding the reason for their visit , their chief complaint, and mechanism of injury ( if there was any) prior to beginning the examinations. Most importantly try to observe for some clues that were discussed earlier that might be apparent before you begin your examination. Also, if you finish early with an examination and there is still time available, make use of the time by asking more questions or going over things you might have left out. Never stop interacting or asking the patient questions once you have finished your examinations even if you are certain you know what the problem or diagnosis may be. The observing doctors grading you also look to see how well you ask questions, what type of questions you ask, and how well you utilized your time. In general, you will need the full five minutes in the physical examination station.
Back to Top of Page
VITAL SIGNS
You may be asked to perform vitals but due to time constraints it is less likely that assessment of the vitals will be asked. However, NBCE has in the past asked students to take the blood pressure. If NBCE does not ask you to take the vitals, they will most likely appear in the patient's additional history section of the post-station (inside the booklet). It should be mentioned once again that in all of the post-stations, you will be given additional information about the patient such as vitals, blood tests, previous injuries, family history, or other important information.
Verbal Component: The observing doctor may ask you to state one of the stages of hypertension.
For example: "What would be stage 2 hypertension?" (In this case, you would need to indicate the numbers/ranges shown below).
Table 1. (Classification of blood pressure levels for adults aged 18 years and older.)
Category |
Systolic blood pressure (mm Hg) |
Diastolic blood pressure (mm Hg) |
Normal |
<120 |
<80 |
Pre-hypertension aka high-normal |
120-139 |
80-89 |
Hypertension—mild--(stage 1) |
140-159 |
90-99 |
Hypertension—moderate--(stage 2) |
160-179 |
100-109 |
Hypertension—severe--(stage3) |
180-209 |
110-119 |
Crisis Hypertension |
>210 |
>120 |
If you are asked to perform the blood pressure, quickly take the blood pressure and state the reading ( Note: Perform this examination last = time consuming ). Also look to see if there is a verbal component with this examination (The verbal component may ask you to state one of the ranges of hypertension. For example: These are possible ways the questions may be asked:
1. “State the ranges of stage 2 hypertension (verbal component) ”
2. "After you take the blood pressure, state your findings (verbal component)."
3. “Take the blood pressure of the patient, state your findings, and state the ranges of severe hypertension (verbal component) .”
Study and memorize the following table below. We have provided the normal results for an adult only. If you'd like, you may also review the normal results for a child and an infant, although it is not recommended.
Table 2. Vital Signs
Examination |
Adult ( Normal ) |
Blood Pressure |
120/80 |
Temperature |
98.6 |
Pulse rate |
60-100 |
Respiratory rate |
14-20 |
NBCE will indicate the type of examination you would need to perform for the Vitals. You will not be asked to perform all of the Vitals.
Back to Top of Page
Eye Examination:
Inspection:
Inspection of the eyes are not usually asked on the Part IV examination. However, you should be careful to observe any abnormalities even though you may not be asked to perform this examination directly. Observe to see if the patient constantly rubs the eyes (itching possibly due to allergies), is wearing sunglasses (photophobia, headaches caused by light sensitivity, eye surgery), is making abnormal eye movements (straining eyes due to bad vision, which could possibly cause headaches) etc.
If asked to perform inspection of the eyes, the following structures/conditions should be emphasized.
- Observe for ptosis, exophthalmia, lesions, deformity, or asymmetry.
- Observe the eyebrows, eyelids, conjunctiva, cornea, sclera, lens, iris, pupils and lacrimal apparatus for any abnormalities.
Below you will find a few important conditions and their findings associated with structures of the eye(s).
Table 3.
Area of concern |
Findings |
Conditions |
| Eyelids |
Drooping(Ptosis)
Inflammation of edges of eyelids, itching, burning, redness, swelling of eyelid edges, sensitivity to bright light. Staph infxn, associated with acne rosacea and seborrheic dermatitis.
Swelling of oil glands of the eyelid due to a blocked duct, usually painless. Looks similar to a stye. Due to a blocked oil duct (the duct becomes blocked and the body continues to produce oil and since it cannot be secreted, it forms a lump.
An infected eyelid gland; painful. Looks similar to a chalazion. It is an infected hair follicle (staph infection)
Flat yellow, white growths on the upper part of the eyelid due to high cholesterol levels
Horner's Syndrome --> miosis, ptosis, and anhydrosis on ½ the face
|
Myasthenia Gravis, Horner's syndrome, Cranial nerve III problem.
Blepharitis
Chalazion
Stye (hordeolum)
Xanthelasma
Pancoast Tumor, Whiplash Accident, TOS
|
Sclera |
Yellow
Red
|
Jaundice
Scleritis, conjunctivitis (common causes consist of collagen vascular diseases, Rheumatoid Arthritis, SLE)
|
Conjunctiva |
Red, inflammation or irritation of conjunctiva. Either viral, bacterial or allergic (however, there are other less common causes). Watery or purulent discharge, mild photophobia.
Pale conjunctiva
|
Conjunctivits aka Pink eye
Anemia
|
Cornea |
Foreign object, scarring, inflammation
Corneal swelling, pain or distortion/impairment of vision.
Cloudy material on the cornea (may or may not produce pain and/or impairment of vision)
Progressive nearsightedness, irregular astigmatism and blurred vision |
Infection (Keratitis)
Fuch's Dystrophy
Corneal Dystrophy
Keratoconus
|
Pupil |
Unequal pupil size
Pupillary constriction
A miotic pupil that responds to accommodation but not to light
A pupil that does not react to light, convergence or accommodation
Dilated pupil |
Anisocoria
Miosis
Argyll-Robertson pupil
Fixed pupil
Adie's pupil
|
Back to Top of Page
Palpation:
Low chance NBCE will ask you to palpate the eyes. In general, we believe if a certain examination is dangerous or risky to perform, NBCE will most likely not want students performing it on patients (Liability Issues). Digital palpation is used to determine elevated ocular pressures primarily due to glaucoma. Know that a “ Tonometer ” is an instrument used to detect intraocular pressure (IOP) and is used to detect the presence of glaucoma.
Instrumentation:
Opthalmoscopic examination will most likely NOT be asked. However, if NBCE asks you to perform an opthalmoscopic examination, make sure that you dim or turn off the lights in the room prior to performing the examination. If you have NOT been instructed to perform the examination, then it is possible that they will ask questions in the post station related to the structures commonly observed with an ophthalmoscope such as the ones listed in Table 4 below:
Table 4.
| Questions |
Answers |
| What is the color of the normal optic disc? |
Yellowish orange to creamy pink |
What is the color of the normal optic cup? |
Yellowish white |
| What is the color and location of the normal macula lutea? |
Yellowish (located lateral to optic disc ) |
| What is the normal cup to disc ratio? |
(1:2 or 0.5 increased ratio indicates glaucoma) |
| Appearance of the optic disc with Papilledema? |
Elevated |
| Appearance of the optic disc with Glaucoma? |
Cupping |
| What setting do you use to asses a papilledema or a glaucoma? |
Slit lamp Fundoscopy |
| What do Arteries look like? |
Smaller, thinner, and lighter (red) |
| What do Veins look like? |
Larger, thicker, and darker (red) |
| What is the Fovea? |
Area of most acute vision |
| What may cause an absent red reflex? |
Cataracts |
| What causes AV-nicking? |
Long standing hypertension |
A penlight is used to detect pupillary function. This testing insures the proper function of the pupils and possible disorders associated with abnormal constrictions or dilations. The light should be shone slightly inferior to superior and not directly into the pupil.
Table 5 below shows the eye examinations/tests used and the structures evaluated.
Table 5.
Tests |
Structures evaluated |
Direct light reflex |
Cranial Nerves II(sensory) and Cranial nerve III(motor) |
Consensual light reflex |
Cranial nerves III in the opposite eye |
Visual Acuity (use a Snellen chart) |
Measures sharpness of sight |
Accommodation |
Cranial nerve III |
Extra ocular movements (trace out the letter H) |
Extra ocular muscles-- Cranial nerves III, IV, VI control movement and cranial nerve II for vision. |
Visual fields |
Checks for normal and abnormal pathways of visual impulses |
NBCE has in the past asked questions related to the eyes in the form of a verbal component. Memorize the muscles, their innervations, and actions as shown in Table 6 and the image below. Know the possible clinical presentations associated with eye muscle dysfunction and possible cranial nerve lesions.
Table 6.
Muscles |
Innervation |
Action |
Superior Oblique |
CN 4 |
Depresses eye in adduction |
Lateral Rectus |
CN 6 |
Abducts eye |
Medial Rectus |
CN 3 |
Adducts eye |
Inferior Rectus |
CN 3 |
Depresses eye |
Superior Rectus |
CN 3 |
Elevates eye |
Inferior Oblique |
CN 3 |
Elevates eye in adduction |
Mnemonic: SO4, LR6, MISI 3 |
|
Back to Top of Page Ear Examination:
Inspection:
Look for symmetry, size, shape, nodules, lesions, scars, swelling, redness, and discharge that may be associated with the patient's condition.
Palpation:
Palpate the ear for tenderness, swelling, nodules, or other abnormalities. Pain upon palpation or pulling of the ear can indicate otitis externa or mastoiditis. If you palpate the tragus or pull the pinna and the patient complains of pain --> think of possible otitis externa. If you palpate the mastoid process and the patient complains of pain it may be due to mastoiditis or otitis media. Prior to palpation, it would be advisable to ask the patient a few questions in order to be certain a patient has an ear problem as opposed to other disorders that may cause pain around the ear. The following questions should be asked:
1. Any discharge from the ear (now or in the past) and if so what color?
2. Any difficulty hearing or changes in hearing?
3. Any ringing/noises in ears?
4. Any pressure inside ear(s)?
5. Any vertigo?
6. Any recent fever?
7. Hearing sensitivity?
8. Any itching inside the ear?
9. Any trauma to the head or ear? |
Note: If the patient answers "NO" to any of the questions above, but complains of ear pain, then you could assume the ear pain is due to one or more of the following conditions (these are indirect causes of ear pain): TMJ disorder, Trigeminal Neuralgia, Dental problems, Sinusitis, Tonsillitis, Bell's Palsy, Neck problems and possibly Temporal Arteritis. If the patient answers "YES" to any of the questions above, then expect the patient to have pain during palpation of the ear or around the ear. By asking such specific questions prior to performing a certain examination, you will be able to more easily and readily identify a problem or condition.
Back to Top of Page
Instrumentation:
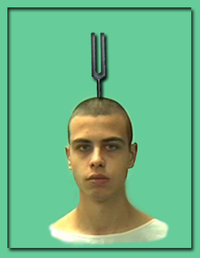
You will most likely NOT be asked to use an otoscope to perform an examination of the ear (only study possible diseases/disorders and structures seen during an otoscopic examination for it may appear in the post station questions). However, NBCE may ask you to use a tuning fork to perform an auditory examination. You will also be required to differentiate between the different types of tuning forks and you must choose the proper tuning fork for the type of examination asked. NBCE may place a few tuning forks and have you choose the correct one for the examination. Remember, the 512 Hz and 256 Hz tuning forks are used for auditory examinations, whereas the 128 Hz tuning fork is used for vibratory testing.

From a clinical point of view, the tests listed below are usually performed if a patient complains of hearing loss. If a patient complains of hearing loss and NBCE does not ask you to perform these examinations then you should NOT perform what is not asked of you (In such situations, you must attempt to take a detailed history to determine the possible cause of hearing loss). Only perform the examinations that are specifically asked by NBCE.
Table 7.
Tests |
Purpose |
Interpretations |
Whisper test/finger rub test/watch test |
Used as a screening test to determine if a patient has a hearing problem.(Also differentiates good ear from bad ear) |
- Diagnosis will be based on the Rinne's and Weber's Tests
|
Weber's test(lateralization test) |
Conduction Vs. Sensorineural hearing loss |
- Sound heard better in the bad ear indicates conduction problem.
- Sound heard better in the good ear indicates sensorineural problem.
|
Rinne's test |
Compares the duration of bone conduction with that of air conduction. (This examination should be done on the bad ear to confirm the findings from the Weber's test) |
Air conduction(AC) should be twice as long as bone conduction(BC)-- (this is called a positive test).
- If BC>AC --- Conductive hearing loss is confirmed with Weber's test (called a negative test).
- If patient hears louder with bone conduction vs. air conduction, then think conductive haring loss.
- If bone conduction and air conduction are both diminished, and air conduction is perceived louder, then sensorineural hearing loss is suggested.
|
Example:
Patient complains of difficulty hearing. Your first step would be to determine which is the “bad ear” by performing one of the screening tests (whisper/watch/finger rub). If NBCE does not ask you to perform the screening test then you should not. In this case, you should have the patient tell you from which ear he or she is having difficulty hearing from and you should then proceed with the Weber's and Rinne's tests.
Give instructions to patients prior to performing the examination(s). Tell the patient what you are attempting to do and what they should expect (This way you are inderectly showing the observing doctor that you understsand how the examination is performed).
- In this case you could say for example:“Now I'm going to perform an examination for auditory acuity. I'm going to place the handle of the tuning fork on top of your head; normally the sound should be heard equally from both ears, please let me know if you hear the sound equally in both ears or louder/better in one ear vs. the other.”
It is very likely that NBCE will make this section/examination into a verbal component.
The objective of these examinations is to determine the following problems:
1. Air conduction hearing loss
2. Sensorineural hearing loss
Table 8. Weber's Test and Rinne's Test
I. Perform the Weber's Test
a. Strike the tuning fork and place the handle on top of the patient's head and have the patient indicate from which ear he or she hears it better in.
1. If patient hears the sound better in the left ear (bad ear), think possible conductive hearing loss.
2. If patient hears the sound better in the right ear (the good ear), then it is likely that the patient has a sensorineural hearing loss in the left ear(bad ear). Now you must perform Rinne's test to confirm.
|
II. Perform the Rinne's Test
Again explain to the patient what you are going to do and what to expect. Hre's an example: “Now I'm going to perform what is called the Rinne's test. I'm going to place the handle of the tuning fork on your mastoid process located behind your ear. When you stop hearing the sound say “stopped”, then I will place the tuning fork next to your ear and I want you to tell me if you are able to still hear the sound. As soon as you hear the sound, say “now”. Then tell me when you stop hearing the sound by stating “stopped” again. If you do not hear the sound simply state “No sound”. Proceed with the examination.
Note: Rinne Positive means that: Air conduction is twice as long as bone conduction.
a. Place the tuning fork on the mastoid process of the bad ear(left) and have the patient indicate when he stops hearing the sound of the tuning fork (step 1). When patient stops hearing the sound, lift the tuning fork off the mastoid process and place it next to the ear (step 2). Normally, air conduction is twice as long as bone conduction.
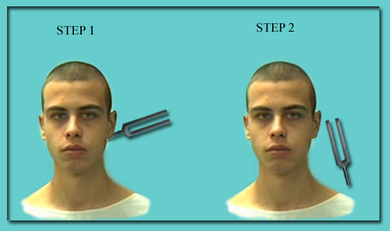
1. If bone conduction is longer than air conduction (BC>AC), think conductive hearing loss; or if the patient can hear louder with bone conduction vs. air conduction, it is also a conductive hearing loss.
2. If both bone conduction and air conduction are significantly diminished (compared to the opposite ear) but air conduction is perceived as louder, then think sensorineural hearing loss.
|
Back to Top of Page
Table 9. The table below shows the etiologies associated with each hearing loss
Conductive Hearing Loss Etiology |
Sensorineural Hearing Loss Etiology |
- Cerumen buildup(ear wax)
- Foreign object
- Infection(otits media or externa)
- Trauma
- Otosclerosis
- Tumor of middle ear
- Perforated or ruptured ear drum
|
- Presbycusis(age related)—most common
- Trauma
- Infections
1. Viral = mumps, measles
2. Bacterial = meningitis
- Labyrinthitis
- Meniere's disease
- Acoustic neuroma
- Repeated continuous loud noise exposure—this tends to damage the hair cells.
- Medications—Some medications cause damage to hair cells in the inner ear and the auditory nerve.
- Strokes
- Brain Tumors
- Multiple Sclerosis
|
Back to Top of Page
In adults, the otoscopic examination is performed by pulling the auricle upward and backward. In children, the auricle is pulled downward and backward.
Note: Cone of light --> The cone of light reflex extends antero-inferiorly from the umbo (in a healthy ear). The Light reflex --> reflects off of the eardrum.
Table 10. Otoscopic examination--- important findings of the ear drum:
Structure |
Findings |
Ear drum (Tympanic Membrane) |
| Normal ear drum |
Pearly grayish and translucent |
| Pink |
Inflammation (myringitis) |
| Angry red |
Infection (otitis media) |
| Red |
Can be due to crying in children or inflammation |
| Light brown, dark brown or orange brown |
Ear Wax |
| White or yellowish |
Collection of exudates(pus), tympanosclerosis or rupture of the ear drum. |
| Straw/Amber |
Serous effusion(serous otitis media) |
| Blue/black |
Due to hemorrhage into middle ear |
| Increased vascularity |
May be due to excessive crying |
| Bulging ear drum |
Acute otitis media |
| Retracted ear drum |
Chronic otitis media |
|
Note: Children are more likely to have Otitis Media and adults are more likely to have Otitis Externa.
Otitis Exerna:
- Otitis Externa (Swimmer's Ear) – Red or moist ear canal. Tenderness of the pinna, tragus or both. Ear pain, itching, discharge, fullness and some hearing loss. Tinnitus and vertigo may also be present.
Otitis Media
- Otitis Media – Infection of the middle ear. Ear pain, fullness, some hearing loss, flu-like symptoms, fever, discharge.
Types of ear discharge (aka Otorrhea)
a. Bloody Otorrhea --- Can be due to trauma, barotraumas, foreign body, rupture of the ear-drum and Cancer.
b. Waxy – Cerumen.
c. Purulent – acute and chronic suppurative otitis media, Otitis Externa (Swimmer's Ear).
d. Non purulent – Otitis Externa (Swimmer's ear), foreign body, Cerebrospinal fluid (CSF) leakage due to trauma.
Back to Top of Page
Nose Examination:
Inspection:
NBCE will most likely NOT ask you to inspect the nose. Although, it is a good idea to know what to look for.
Observe the size and shape of the nose. Look for any deformities, previous fractures, a deviated nose/septum, ulcerations, skin disease, scars, cuts/creases, swelling, redness or discolorations, discharge and unpleasant smell.
Palpation:
NBCE will most likely NOT ask you to palpate the nose.
Palpation is used for assessing any pain or tenderness, swelling, crepitus, deformities, nodules etc.
Instrumentation:
NBCE will most likely NOT ask you to use the Otoscope, speculum or other forms of instrumentations to examine the nose. NBCE however can ask you to perform “sense of smell” examination.
Examination: “Sense of smell”
The patient will most likely complain of a stuffy nose, difficulty smelling, or differentiating taste of foods. A patient might also complain of headaches or pain in the face. It would be your objective to find why the patient would have the following problems. Again explain to the patient prior to beginning the examination what you are attempting to do. NBCE will likely have two or more different odors for you to choose from. Make sure you use a different odor for each nostril. Have the patient close both eyes. Then ask the patient to close one of the nostrils and ask him or her to identify the odor as the odor is brought closer to the nose. Then switch to another odor, have the patient close the nostril that was previously tested and have the patient again identify the new odor with the eyes closed again. Difficulty smelling or identifying the type of odor can suggest the following:
Sinus related problems, growths in the nasal passages, brain tumors, deviated nasal septum, nasal polyps, upper respiratory infections, irritants such as cigarette smoke or pollutants or drug addictions such as cocaine, allergies, trauma to the head, occupational exposure to chemicals, or simply due to old age.
It would be your objective to find out when the problem started, how long they've had this problem, what the patient was doing at the time, and some possible associated symptoms. For example:
Patient complains of headaches and NBCE has asked you to check the patient's sense of smell along with other orthopedic/neurological examinations. The test revealed that the patient cannot smell from either nostril. Since the primary complaint was headache, you must have a few differentials that would cause a headache and also cause the patient to have loss of smell. Sinus related problems, a recent illness, infection, possible stroke , tumors, trauma to the head are possible differentials that can cause headaches and loss of smell. The following questions should be asked:
1. Any sinus related problems or pain in your forehead, under the eyes or around your face? (possible sinus related problems)
2. Do your headaches wake you up at nights, cause any changes in vision nausea or vomiting? Have you noticed any confusion? (possible brain tumor)
3. Any history of trauma to the head, face, or nose?(brain injury, broken facial bones, or nasal bone.)
4. Any recent fevers or sicknesses? (possible upper respiratory infection)
5. Also ask about family history of Alzheimers, Parkinsons's, Epilepsy and Multiple Sclerosis, etc. |
The questions mentioned above can help you porperly diagnose the patient. Ask detailed questions and try to expand upon each answer. If you do no ask the patient questions during the examination, you will have difficulty answering the questions in the post stations.
Back to Top of Page
Mouth and Throat Examination:
Inspection
NBCE will most likely NOT ask you to do an inspection of the mouth or throat. However it would be important to note the following structures assessed during an inspection of the mouth and throat.
Inspect the color of the lips and note for moister (normal), lumps, cracks, dryness, lesions or other abnormalities (erythema or leukoplakia, cold sores (HSV-1), angular cheilitis etc.). If NBCE gives you a tongue depressor, you should definitely use the device to assess the inside of the mouth and throat. If NBCE also places gloves and a penlight, you should use both during the examination. Always be aware of the tools/instruments NBCE places in the room and use good judgment upon choosing these tools for the examination. Also if a sanitizer is placed in the room, always use it before you assess the patient. Next, check the following structures:
1. Buccal mucosa – color, lesions, ulcers, bumps etc.
2. Teeth and gums – swelling, bleeding, discoloration, dryness, missing teeth, and dental problems (tooth abscess) or abnormalities.
3. Tongue – cracks, fissures, coating, discolorations, symmetry, texture, lesions.
4. Palate – lumps/elevations, color changes, lesions
5. Uvula - Note that the uvula is hanging straight down and is directly in the mid-line.
6. Tonsils – present or absent, color, size, symmetry, white or yellow discharge |
Palpation:
Palpation of the mouth will most likely not be asked.
Instrumentation:
NBCE may ask you to use a tongue depressor or a penlight to assess the inside of the mouth, tongue and throat. Remember to quickly check each of the structures listed above and try not to spend too much time in this section. Quickly ask the patient if they have any pain/discomfort, bleeding, difficulty/pain with chewing, or tasting foods prior to examining the patient. If patient answers "NO" to any of the above, quickly perform this examination and move on to the next examination.
- Also have the patient stick their tongue out for evaluation of the Cranial Nerve 12 (note: tongue always deviates toward the side of lesion).
- The uvula always deviates away from the side of lesion when patient says “ahhhhh” (assesses cranial nerve # 10).
- Gag reflex requires a sensory component (CN 9--Glossopharyngeal Nerve) and a motor component (CN 10 --Vagus Nerve).
Back to Top of Page Sinus Examination:
Inspection:
Observe the areas of the sinuses for redness, bumps, swelling, asymmetry etc.
Palpation:
NBCE may ask you to palpate the frontal and maxillary sinuses. Again, tell the patient what you're going to do and ask them to tell you if they experience any pain (usually due to inflammation if trauma is ruled out) during palpation of the sinuses. Tell the patient that normally you will feel some pressure but you should not feel pain. Also ask the patient if they have or have had a recent fever, nasal congestion, facial pain and discharge, which could suggest a sinus related problem.
In addition, ask the patient how long they've had these symptoms in order to differentiate between acute vs. chronic sinusitis. (If recent = acute sinusitis; if patient has a reoccurring problem or has had the problem for a long time = chronic sinusitis)
Differentiating whether patient has a frontal or maxillary sinus related problem.
Table 11.
Frontal Sinusitis |
Maxillary Sinusitis |
a. Headache in the forehead.
b. May be unilateral or bilateral.
c. Pain with bending or stooping.
d. Pain over the forehead with palpation of the frontal sinuses.
e. Symptoms are worse when lying on the back(reclining).
f. Symptoms are better when the head is upright.
g. Nasal discharge or postnasal drip. |
a. Pain around the cheeks, eyes, or upper teeth.
b. May be unilateral or bilateral.
c. Ache in the upper jaw, upper teeth and at times in the hard palate.
d. Redness, swelling, and tenderness over the cheekbone area and sometimes around the eyes.
e. Symptoms are worse when the head is upright or while bending forward;
f. Symptoms are better when patient reclines.
g. Nasal discharge or postnasal drip. |
Instrumentation:
NBCE may ask you to perform transillumination of the sinuses. You will only need to perform transillumination of the frontal and maxillary sinuses. Make sure you dim the room light or turn off the light prior to beginning the examination. You will need to choose the otoscope for this particular examination. Look to see if the sinuses light up symmetrically. If you are asked to perform this examination, the patient will most likely not have an observable decreased light transmission. Decreased light transmission is indicative of sinusitis.
Percussion:
Percussion of the sinuses. It should be noted that this examination is not usually asked. Simply learn how to perform this technique incase it is asked.
Back to Top of Page
Neck Examination:
You will most likely be asked to perform the following examinations under this section:
1. Palpation of the lymph nodes of the head and neck.
2. Palpation of the thyroid gland.
Inspection:
Inspect the neck for asymmetry, swelling, scars, lumps, cuts, bruises, rashes, lesions, distension of veins etc.
Palpation:
1. Lymph nodes
- Palpation of the lymph nodes.
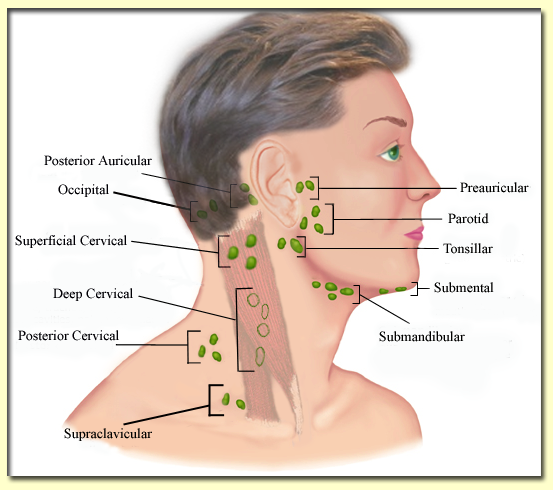
-NBCE may ask you to palpate and name the following lymph nodes as a Verbal Component.
Table 12. Lymph Nodes of the Head and Neck
1. Occipital
2. Posterior auricular
3. Preauricular
4. Tonsillar
5. Parotid
6. Submandibular
7. Submental
8. Superficial cervical
9. Posterior cervical
10. Deep cervical
11. Supraclavicular |
|
Know the difference between an infected lymph node and a malignant lymph node as shown in Table 13:
Table 13. Infected vs. Malignant Lymph Nodes
Infected Lymph Nodes |
Malignant Lymph Nodes |
- Soft
- Tender
- Enlarged
- Warm
- Mobile(freely movable)
- Associated fever
|
- Firm or rubbery
- Non-tender
- Stuck to one another(matted)
- (Immobile) not freely movable
- Increase in size over time
- Associated weight loss
|
Back to Top of Page
Table 14. Lymphadenopathies
| Type of Lymphadenopathy |
Symptoms/Characteristics |
| Hodgkin's Lymphoma |
- Affects individuals between 15-35 years of age and adults over 50 years of age.
- The Cancer cells are called Reed-Sternberg cells(B-Lymphocytes)
- Cancer of the lymphatic system.
- Painless swelling of lymph nodes in groin, armpits, and neck regions
- Fever with possible chills, night sweats, weight loss, flu-like symptoms, fatigue.
|
| Non-Hodgkin's Lymphoma |
- Same signs and symptoms as in Hodgkin's Lymphoma.
- Difference between Hodgkin's and Non-Hodgkin's Lymphoma is in the types of lymphocytes involved (Non-Hodgkin's Lymphomas do not involve the Reed-Sternberg cells, which are associated with Hodgkin's Lymphoma ).
|
Leukemia
4 types of Leukemia:
a. Acute Lymphocytic Leukemia (ALL)
b. Chrnoic Lymphocytic Leukemia (CLL)
c. Acute Myelogenous Leukemia (AML)
- Average onset is 65 years of age
d. Chronic Myelogenous Leukemia (CML)
- Average onset is 65 years of age
|
1. Acute Lymphocytic Leukemia (ALL)
(aka Lymphoblastic or Lymphoid leukemia.)
- Children under age of 10.
- Most common leukemia in children.
- Affects immature blood cells not mature
- Affects group of white blood cells called Lymphocytes.
- May also occur in adults.
2. Acute Myelogenous Leukemia (AML)
(aka Granulocytic, Myelocytic, Myeloblastic or Myeloid Leukemia.)
- Occurs in adults mostly (average age of onset is 65) but can occur in all age groups.
- Most common leukemia in adults.
- Affects group of white blood cells called myeloid cells (granulocytes or monocytes).
- Affects immature blood cells not mature.
- Does NOT affect the lymphocytes
***************************************************************
Symptoms for all types of leukemia are similar:
- Anemia, Fever, chills, nosebleeds, bruising easily, loss of appetite, tender-swollen lymph nodes, splenomegaly, hepatomegaly, bone or joint pain, abdominal distress.
|
Infectious Mononucleosis
(Glandular Fever) |
- Caused by Epstein-Barr virus
- Significant fatigue, fever, sore throat, swollen lymph nodes in neck, throat, armpits and groin. May present with splenomegaly or hepatomegaly.
- The disease is self-limited.
- Diagnostic Test: + Monospot Test ( Heterophile antibody test) --> IgM heterophil antibodies are detected
Note: If mononucleosis is due to CMV, then monospot test will be negative and hepatosplenomegaly will likely not be seen. Therefore, to rule out CMV you should perform the following tests: CMV ELISA antibody test and CMV serum PCR test.
|
| Human Immunodeficiency Virus (HIV) |
Fever, unexplained weight loss, night sweats. Swollen lymph nodes in the neck, armpits, and groin. Swollen glands. Flu-like symptoms, muscles aches, fatigue, appearance of purplish lesions on the skin (can even show up in the mouth).
Prone to the following opportunistic infections:
1. Candidiasis(Thrush)
2. Cytomegalovirus (CMV)
3. Mycobacterium Avium Complex (MAC)
4. Pneumocystis pneumonia (PCP)
5. Tuberculosis
6. Toxoplasmosis
7. Herpes Simplex and Herpes Zoster virus
8. Kaposi's Sarcoma
9. Lymphoma
|
Back to Top of Page
2. Thyroid gland
Inspection of the thyroid gland:
Patient should be sitting comfortably with the neck slightly extended.
Look for symmetry, swelling and enlargement. An enlarged visible thyroid is called Goiter.
- Have the patient swallow a sip of water (if a cup of water is provided), and watch how the thyroid gland moves up and down. Movement should be nice and smooth.
Palpation of the thyroid gland:
It should be noted that it is possible that NBCE may ask you to palpate the thyroid gland; however, it is too close to the carotid arteries and NBCE may not want students palpating near it. Therefore, it is a risky examination and most likely will not be asked. It is however recommended that you should know how to perform the examination.
- Note the size and symmetry. Normally, the thyroid gland should move freely upon swallowing. Also observe for any nodules. Observe to see if the thyroid gland is firm and if it is attached to surrounding structures which could indicate malignancy.
Remember: associated signs and symptoms along with the patient's blood results and history will help you diagnose the true type of thyroid problem.
Table 15. Below you will find a list of important thyroid conditions and their clinical presentations/symptoms
Thyroid conditions |
Clinical Presentations/Symptoms |
Hyperthyroidism |
Heat intolerance, weight loss, frequent sweating, warm skin, frequent and loose bowel movements, weight loss with normal eating habits, tremors, irregular heart beat, nervousness.
|
Hypothyroidism |
Weight gain, Loss or thinning of eyebrows, Cold intolerance, Low sex drive, Cold hands or feet, Dry or thinning hair, puffy face, depressed, cold skin, dry skin, feeling tired or weak, memory problems and constipation.
|
Goiter |
Swollen in front of the neck(enlargement of the thyroid gland), difficulty breathing, swallowing and wheezing if goiter is large enough and puts pressure on the trachea
|
Hashimoto's disease/Thyroiditis |
Autoimmune disease, gradual destruction of the thyroid gland --> eventually causes hypothyroidism. Pyramidal lobe enlargement and firm thyroid (goiter), difficulty swallowing, breathing. Signs and symptoms of this disease are similar to that of hypothyroidism. Lab findings = increased antibodies against thyroglobulin (TG) and thyroid peroxidase (TPO), which is not the case with hypothyroidism. Goiter is also a characteristic of Hashimoto's. |
Grave's Disease |
Autoimmune disease which causes an overactive thyroid gland. Symptoms are similar to that of Hyperthyroidism but patients with Grave's disease also have at least one of the following:
- Bulging eyes (exophthalmos)
- A diffuse goiter
- Pretibial myxedema (raised, reddish thickening of skin in front of the shins).
|
Thyroid Tumor (Malignant) |
Small nodules, lumps, hoarseness, enlarged lymph nodes in the neck area, pain in throat region, sore throat, difficulty breathing, eating or even speaking, unintentional weight loss.
Note: majority of the lumps or nodules in the neck are benign only a small percentage are malignant.
|
Thyroid Nodules |
Over 90 percent of nodules in the thyroid are benign and do not cause problems, especially if they are found to be Hot on thyroid scan. |
Back to Top of Page
Lung Examination:
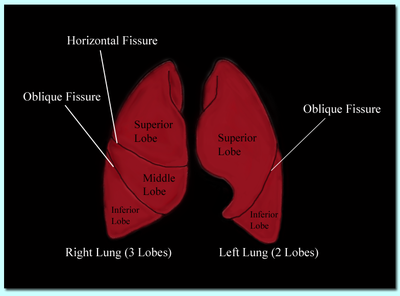
The left lung has 2 lobes (Superior/Upper and Inferior/Lower); the right lung has 3 lobes (Superior/Upper, Middle, and Inferior/Lower). The right lung is slightly larger than the left lung.
Review and familiarize yourself with the following terms which may show up in the post station questions:
Breathing related problems:
- Apnea: Cessation of breath.
- Bradypnea: Slow breathing rate.
- Tachypnea: Rapid, shallow breathing.
- Hyperpnea: Rapid, deep breathing; hyperventilation.
CHEYNE-STOKES RESPIRATION: Is defined as repeated alternations between cessation of breath (apnea) and rapid deep breathing (hyperpnea).
Associated Conditions:
• Congestive Heart Failure (CHF)
• Uremia
• Meningitis
• Pneumonia |
• Brain Tumor
• Brain Injury
• Stroke
• Coma |
Inspection:
Observe the patient's chest and respiration (rate, rhythm, depth, effort of breathing, and sound of breathing.) Normal rate of breathing is 14-20 breaths/minute .
Also look for any masses, lesions, scars, bruises, deformities, nodules, swelling, etc.
As you begin the examination look to see how the patient is breathing (note the rate and rhythm, depth, effort of breathing and if patient is making any sounds such as wheezing while breathing). There are only a few symptoms the patient can "act out" to demonstrate that he or she may have a lung related problem such as wheezing, coughing, breathing rapidly, heavy breathing, stating he or she has pain with breathing, etc.
Note: The patient will likely be complaining of chest pain and it will be your responsibility to determine whether the patient has a lung or heart condition or other disorders that may cause chest pain (rib or sternal fracture, hiatal hernia, anxiety, peptic ulcer, aortic dissection etc.) - The positive or negative findings based on the examinations NBCE asks you to perform and the type of questions you ask the patient during the course of the examination will determine what kind of a problem the patient may have (additional history and x-ray findings in the post-stations will also assist you). It is highly advisable that you ask detailed questions in order to help you differentiate one condition from the other. Review the table below for associated symptoms of the lungs and heart.
Table 16. Symptoms of Heart and Lung Disease
Important Symptoms of Lung Disease |
Important Symptoms of Heart Disease |
Coughing |
Palpitations |
Wheezing |
Lightheadedness, Dizziness |
Dyspnea |
Sweating |
Hemoptysis |
Nausea |
Cyanosis |
Radiating pain into arm, jaw, neck or back. |
Chest pain |
Chest pain (pressure, heaviness ) |
Hoarseness |
Weakness, anxiety or shortness of breath |
Mucus production |
Tiredness/Fatigue |
Back to Top of Page
Palpation:
Highly possible that you may be asked to perform Tactile Fremitus and Chest Expansion/Excursion. Tactile Fremitus aka Vocal fremitus: (Verbal Component). Used to assess the types of vibrations generated with speech. The front and back of the chest should be assessed with this examination. Also, both sides (right and left) of the chest and back should be assessed simultaneously using the ball of your hands. Compare both sides as the patient repeats “ninety-nine” or “eee”. The observing doctor may ask you to state a condition that causes increased fremitus and a condition that cause a decreased fremitus.
- As a general rule, consolidation causes increased tactile fremitus caused by Lobar Pneumonia. Pneumonia is the ONLY condition which causes increased tactile fremitus. All other conditions will cause decreased tactile fremitus (Pleural effusion, Pneumothorax, COPD etc). This might show up in the post-station questions or as a verbal component in a pre-station.
Chest expansion/excursion: (Verbal Component). Assesses symmetry of chest expansion with deep inspiration. Indicate out loud as you are performing the examination that you are looking for symmetry upon deep inspiration and expiration. If the doctor asks you to name 3 causes of decreased chest expansion, simply memorize and answer a few of the causes listed below. The patient can actually alter the expansion of the chest and make it seem asymmetrical upon breathing. Therefore, be cautious as you perform this examination. Also ask to see if the patient experiences pain during this examination and during breathing, which could suggest a possible fractured rib(s), compression fracture, neuralgia or even pleuritis.

Roll your mouse pointer over the image to see action
Note: Many lung diseases and other conditions may cause a decrease in overall chest expansion such as: Bronchial obstruction, hemothorax, myasthenia gravis, pleural effusion, pneumonia, pneumothorax, pulmonary embolism, flail chest (due to rib fractures), paralyzed hemidiaphragm and ankylosing spondylitis. Please make a note of these conditions.
Percussion: (Verbal Component)
Interpreting findings on percussion of the chest: The patients will not have abnormal findings therefore, you may be asked to describe what you are looking for during percussion of the chest in the form of a verbal component. You may want to indicate that normal lung sounds are resonant, and also state what abnormal lung sounds would sound like during percussion as described in table 17 below.
Table 17.
Pathological Lung Conditions |
Findings |
Normal Lung or Bronchitis |
Resonance |
Consolidation(lobar pneumonia), pleural effusion |
Dullness |
Emphysema;
If on one side of the chest think pneumothorax |
Hyperresonant |
Pneumothorax |
Tympanic |
| |
Back to Top of Page
Diaphragmatic Excursion: Usually performed when breathing is shallow and the examiner is suspecting that something could be limiting the movement of the diaphragm.
Decreased or asymmetric diaphragmatic excursion may indicate paralysis, emphysema or broken ribs . (Normal diaphragmatic excursion = 5-6 cm)
Have the patient fully exhale and hold their breath. At this point you would begin percussing (superior to inferior), starting from the lungs posteriorily untill dullness is heard. You would mark this point of expiratory dullness. Then you would instruct the patient to inhale fully and hold their breath. You would then continue to percuss downward from the first marking (expiratory dullness) untill dullness is heard again. Mark the area of inspiratory dullness. Lastly, measure the distance between expiratory and inspiratory levels of dullness. Repeat this process on the other side. (Normal diaphragmatic excursion = 5-6 cm)
Auscultation:
You will be given a stethoscope to perform auscultation of the lungs. Make sure you do NOT perform auscultation over the patient's gown or clothing. Always ask the patient's permision prior to raising or removing the gown for such examinations. Use the diaphragm to listen to the breath sounds. The diaphragm is the big flat shaped part of the stethoscope and the bell is the small cup-shaped part of the stethoscope.
(If you are having difficulty distinguishing the bell from the diaphragm, just remember that a bell looks like a cup and a diaphragm is flat )
Note: If your stethoscope is one sided and does not have a bell or a diaphragm, you must use light touch and hard touch to activate the bell or the diaphragm respectively.
- Press Lightly for Low pitched sounds (Lightly = Low)
- Press Hard for High pitched sounds (Hard = High)
|
|
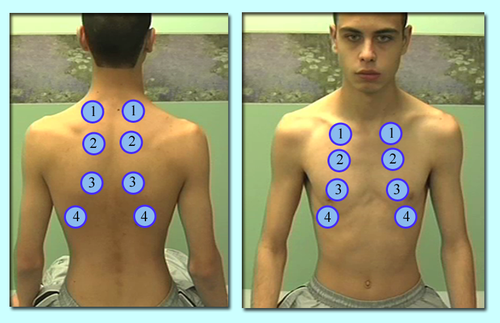
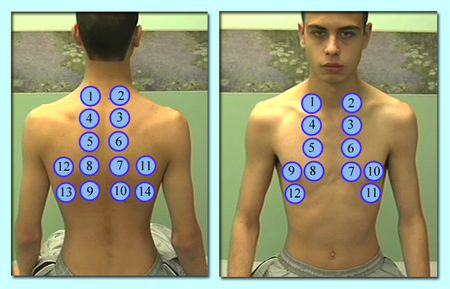
Auscultation of the Lungs
It is highly likely that you will be asked to perform this examination in the form of a verbal component. It will state “perform auscultation of the lungs and identify the lobes of the lungs (verbal component)” or it may state, “auscultate and identify the lobes of the lungs (verbal component).” Your job would be to simply auscultate the lungs and state which lobe you are auscultating during the examination. During the end, simply state that your findings were normal unless the patient was coughing, wheezing or creating an abnormal sound during the examination. It should be noted that most cases will be normal (the patient will not attempt to create an abnormal sound or an abnormal sound will not be present). You should avoid auscultating over the scapulae. The Auscultation points are shown below.
Breath sounds:
Breath sounds are classified into two categories: normal or abnormal (adventitious).
Table 18. Breath Sounds
Type of sound |
Respiratory Cycle |
Areas heard |
Vesicular |
Inspiration > Expiration (I > E) |
Most of lung fields |
Bronchovesicular |
Inspiration = Expiration (I = E) |
- Between the scapulae(posteriorly)
- 1 st and 2nd intercostal spaces anteriorly
|
Bronchial |
Inspiration < Expiration (I < E) |
Over the manubrium |
Tracheal |
Inspiration = Expiration (I = E) |
Over the trachea |
Table 19. Causes of decreased, absent, and unequal breath sounds
| Causes of decreased breath sounds |
Pleural effusion, hemothorax, empyema (pus accumulation in lungs), emphysema, increased thickness of chest wall/pleural thickening. |
| Causes of absent breath sounds |
Pneumothorax and atelectasis |
| Causes of unequal breath sounds |
Pneumonia (consolidation), Lung tumor, atelectasis, foreign body obstruction. |
Back to Top of Page Adventitious sounds: (Abnormal sounds)
Adventitious sounds are those sounds that are NOT normally heard and refer to extra or additional sounds that are heard over normal breath sounds.
Table 20. The four adventitious sounds
Continuous |
Discontinuous |
Wheezes – High pitched, hissing quality.
Causes: Asthma (aka reactive airway disease), chronic bronchitis, obstructing mass (i.e cancer, foreign body in airway). |
Crackles(Rales) – Intermittent and non-musical (rattling or velcro kind of sound).
Causes: Pneumonia, atelectasis, acute and chronic bronchitis, Interstitial lung diseases and pulmonary edema due to left sided congestive heart failure.
|
Rhonchi —Low pitched , snoring quality.
Causes: Asthma, bronchitis, emphysema pneumonia, bronchiectasis, ARDS (Adult Respiratory Distress Syndrome).
Caused by airway narrowing and secretions of the airway. |
Pleural Rubs
Causes: Pleurisy, pleural effusion, pneumothorax. |
Again, for more information regarding lung sounds you may visit the following websites provided below and download or play normal and abnormal lung sounds:
(
CNBA is in no way affiliated with these websites) 1) http://www.stethographics.com/main/physiology_ls_introduction.html
2) http://faculty.etsu.edu/arnall/www/public_html/heartlung/breathsounds/contents.html
Back to Top of Page
Transmitted Voice Sounds:
1. Bronchophony
2. Whispered Pectoriloquy
3. Egophony
Note: Generally, if you hear adventitious (abnormal) sounds where they should not be heard with auscultation, you should then listen for transmitted voice sounds. Normally lungs are filled with air. Air is not a good transmitter of sound, therefore these sounds suggest that air filled lungs have become airless.
Note: The auditory changes listed below may be present if there is consolidation, pleural effusion, infection, tumors or any type of congestion in the lungs.
Table 21. Transmitted Voice Sounds
Bronchophony |
- Instruct the patient to say "99" a few times with a normal voice.
- Normally the sounds you hear during auscultation should be unclear and vague. Bronchophony is present if these sounds are heard louder and clearer than normal.
|
Whispered Pectoriloquy |
- Instruct the patient to “whisper” "1, 2, 3" a few times.
- Normally faint sounds should be heard. Whispered pectoriloque is present if these sounds are heard louder and clearer and distinct.
|
Egophony |
- Instruct the patient to say "e" continuously.
- Normally, you should hear an "e" sound (as in “feet”). When “e” sounds like "a" (as in “day”) and has a nasal sound to it, it is referred to as an egophony.
|
Table 22. Important Lung Diseases
Lung Disease |
Signs & Symptoms |
Causes |
COPD
(Chronic Bronchitis and Emphysema) |
Chronic productive cough, Excessive Mucus Production, Increased shortness of Breath (dyspnea), Wheezing, Chest Tightness, Barrel chest, Cyanosis, Pursed-lips. |
Cigarette Smoking or exposure to cigarette/tobacco smoke is primary cause, Industrial Dusts and Chemical Fumes, Air Pollution, Severe Lung Infections. |
Pneumonia
(Typical Pneumonia or Community-acquired pneumonia) |
Dry or productive cough(later stages)--> Purulent productive cough or blood-tinged sputum. Fever and chills, shortness of breath or wheezing, chest pain with or without breathing, tachypnea, tachycardia, |
Viral or bacterial
-- Streptococcus pneumoniae (most common cause)
Other causes: patient may get Pneumonia following an upper respiratory infection (cold or flu secondary to viral infection) |
Asthma
Younger individuals but can occur in adults
Majority below age 30 |
Wheezing, chest tightness, unproductive cough, shortness of breath(dyspnea), disturbed sleep due to shortness of breath.
Symptoms of an attack
Coughing that won't stop, severe wheezing, shortness of breath, chest pain or tightness, nasal flaring, rapid breathing, difficulty talking. |
Allergens (pets, pollen, food additives(sulfites), house dust and molds).
Irritants (Cigarette smoke, cold air, dry air, pollution, odors such as from paint or scented products, chemical fumes
Other (emotional stress, exercise, and certain medications)
|
Emphysema
(one of a group of lung diseases called COPD)
Over age 40 |
Progressive condition, Shortness of breath, fatigue, wheezing, fast but shallow breathing, coughing with or without sputum, weight loss, cyanosis, excess mucus production, clubbing of fingernails, blue lips, Barrel chest(chronically over-inflated with air).
Note: Usually have shortness of breath and later develop a cough and sputum during a respiratory infection or in later stages of the illness. |
Smoking (primary cause),
Other causes:
2 nd hand smoke, air pollution, chemical fumes, Industrial dusts, severe lung infections, Alpha-1 antitrypsin deficiency(genetic) |
Bronchitis(chronic)
(one of a group of lung diseases called COPD) |
Progressive condition. Persistent cough (with mucus) present majority days of the month, or for 3 months of the year for 2 years in a row without any other underlying diseases that can explain the cough. Persistent cough, Excessive amounts of mucus, clubbing of fingernails, frequent respiratory infections, blue lips and skin, swelling of the feet.
Note: Before these patients develop shortness of breath, they have had a cough and sputum production for several years. |
Smoking(primary cause)
Other causes:
Air pollution, chemical fumes, industrial dusts, constant exposure to smoke from burning structures. |
Pneumothorax
(air escapes from the lung and goes into the pleural cavity, which causes collapsed lung)
|
Sudden sharp chest pain and sudden shortness of breath, rapid heartbeat, cyanosis, tightness in the chest |
Trauma to the chest, broken ribs, barotraumas, COPD, asthma, pneumonia, or spontaneously(spontaneous pneumothorax) |
Pulmonary Embolism |
Sudden sharp, stabbing chest pain. Worse when taking in a deep breath, sweating, fainting/passing out/light headedness, Anxiety, coughing(may produce blood), tachypnea, tachycardia, fever, edema in the leg(s), pleural friction rubs, |
Most common = Blood clot, usually from the leg or in the pelvic region.
Other causes:
--Prolonged sitting
--Trauma in the legs (can cause an embolus to break and travel to the lung)
--Fat embolism after a fracture |
Atelectasis (collapsed lung ) |
Acute : chest pain, dizziness, cyanosis, difficulty breathing, increased temperature, decrease in blood pressure, rapid heart rate(tachycardia)
Chronic : Gradual weakness and dyspnea |
obstruction of small or large lung air passages. Few causes:
-- Tumors that can cause pressure on airways, foreign inhaled objects, chest trauma and fractured ribs, penetrating wound, enlarged lymph nodes. |
Pleural Effusion |
Chest pain, dry cough, shortness of breath, rapid breathing |
Cancer (lung or breast), congestive heart failure, pericarditis, liver disease, tuberculosis, sarcoidosis, mesothelioma, pulmonary embolism, bacterial pneumonia, lung infections, drug reactions, asbestosis, lymphoma and trauma. |
Back to Top of Page
HEART EXAMINATION
Inspection:
Have the patient lie supine (facing up) on the table (Normally the trunk of the patient should be raised 30-45 degrees, but chiropractic tables cannot be lifted and therefore you should not be concerned about raising the patients trunk during this examination). Stand on the RIGHT side of the patient. Observe the precordium (external surface of the body overlying the heart and the chest) and look for any masses, scars, lesions, tachycardia, tachypnea, palpitations, cyanosis, discolorations. Look tangentially and note the location, diameter, amplitude and duration of the apical impulse (aka PMI = Point of Maximum Impulse). Also observe the chest for pectus excavatum (sunken or caved in breast bone) and pectus carinatum (aka pigeon chest --> protrusion of the chest over the sternum)
You may be asked to locate and identify the apical impulse (verbal component). In this situation you must give the actual location of the apical impulse and state how you would locate it. You must state, “Apical Impulse is located at the left 5th ICS (Inter-Costal Space) along the midclavicular line (MCL)”; then, locate the area on the patient.
Note: Normal pulsations of the apical impulse should be noted at the apex in the 5th left intercostal space. Also, you must use “tangential lighting”, which allows movements to be more visible as you observe the apical impulse.
The table below shows a few facts about the Apical Impulse.
Table 23.
Normal Apical Impulse |
Abnormal/Displaced Apical Impulse |
- Located at the left 5th-intercostal space along the midclavicular line
- No more than 2-3cm in diameter
- Very faint
- Not visible in all individuals (due to obesity, heavy chest, COPD etc.)
- Single systolic outward motion
|
Left Ventricular Hypertrophy – Apical impulse is displaced lateral to the midclavicular line and inferiorly; or if diameter of impulse exceeds 2-3cm.
Right Ventricular Hypertrophy – Impulse displaced anteriorly and inferiorly. |
Back to Top of Page
Palpation:
NBCE can ask you to palpate the apical impulse (point of maximum impulse) on the patient and indicate whether it is present or absent). This can also be in the form of a verbal component.
Percussion:
Percussion of the heart may indicate a possible enlarged heart or pericardial effusion. Percussion of the heart produces a dull sound (dullness). As you perform this examination, you will not objectively find that the heart is enlarged or the patient may have pericardial effusion. In this case, the patient may state that he or she is having pain during percussion, which can indicate an underlying problem and a possible enlarged heart. You must also ask specific questions to rule out a possible rib fracture, which could also produce pain with percussion. Remember, if NBCE asks you to perform an examination, which is used to detect a specific condition, the examination findings alone will not always confirm the presense of that particular condition. Therefore, your diagnosis for that condition will be based on the specific types of questions that you will need to ask the patient. Note: NBCE may ask this examination in the following ways: Perform percussion of the heart, or Perform percussion of the heart and state your findings (verbal component).
Auscultation:
Auscultation of the heart is commonly asked by NBCE. NBCE will ask you to either auscultate a specific area of the heart such as the aortic valve, or have you auscultate the valves of the heart:
1. Aortic valve
2. Pulmonic valve
3. Tricuspid valve
4. Mitral valve |
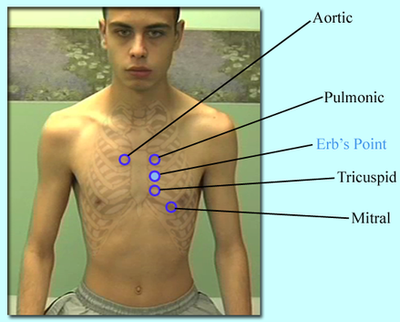 |
Auscultation of the Erb's point may also be asked (used to rule out right sided heart pathologies).
Know the normal heart sounds (S1 and S2) and understand what each one represents:
Note: Normal heart sounds are produced by closure of the valves of the heart.
Table 24.
| S1 = closure of the Tricuspid and Mitral valves (Atrioventricular Valves = AV) |
S2 = closure of Aortic and Pulmonic valves (Semilunar Valves) |
- The 1st heart sound heard (“LUBB”)
- Heard loudest in the Mitral area
|
- The 2nd heart sound heard (“DUBB”)
- Heard loudest in the Aortic area
|
Back to Top of Page
Table 25. The table below shows the structures/areas of the heart and their locations:
Structures/Areas of the Heart |
Location |
Aortic valve (S2) S2 loudest here |
2nd right intercostal space (ICS ) at the parasternal line |
Pulmonic valve (S2) |
2nd left intercostal space (ICS ) at the parasternal line |
Tricuspid valve (S1) |
4th left intercostal space (ICS ) at the parasternal line |
Mitral valve (S1) S1 loudest here |
5th left intercostal space (ICS ) (Apex) at the midclavicular line |
Erb's point |
3rd left intercostal space (ICS ) at the parasternal line |
|
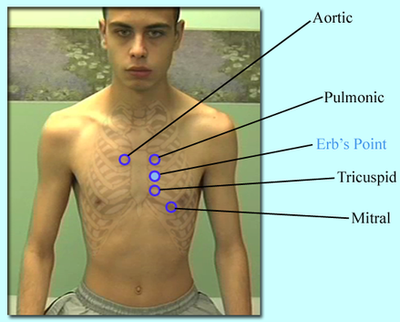 |
Here are a few ways you may be asked to auscultate the heart: (we'll use the Aortic valve as an example)
1. Auscultate the Aortic valve
2. Auscultate the Aortic valve and state its location (verbal component)
3. Auscultate the valves of the heart
4. Auscultate the valves of the heart and state their locations (verbal component)
5. Auscultate the heart (in this case you will have to auscultate all 4 valves of the heart) |
Note: If you are asked to auscultate a specific valve (one valve only), you should perform the examination in the following manner:
(These are known as special maneuvers/positioning).
Table 26. Special Maneuvers
| Valve |
Instructions |
| Aortic |
Have the patient lean forward, exhale fully and hold the breath.
- Use the Diaphragm of the stethoscope
- Used to detect Aortic regurgitation
|
| Pulmonic |
Have the patient lean forward, inhale fully, and hold the breath.
- Use the Diaphragm of the stethoscope
- Used to detect Pulmonary regurgitation
|
| Mitral |
Have the patient roll unto his or her left side (left decubitus position)
- Use the Bell of the stethoscope and listen at the apex.
- Used to detect Mitral stenosis, S3 and S4
|
Back to Top of Page
Table 27. Common Heart Conditions: Signs and Symptoms
Heart Disease |
Signs & Symptoms |
Causes |
Angina |
Stable Angina:
Chest pain, chest discomfort such as tightness. Chest pain worsens with exertion and improves with rest and Nitroglycerines. Chest pain usually lasts about 2-5 minutes (Brief). Radiation of pain into left arm and neck.
Unstable Angina:
Chest pain usually occurs while patient is at rest or during sleep or with NO exertion. The chest pain usually comes as a surprise and lasts longer --> 30 minutes. Not relieved with rest. |
Reduced blood flow to an area of the heart muscle due to narrowing of the arteries (buildup of plaque). smoking, high cholesterol, high blood pressure, diabetes. Chest pain that occurs with physical exertion (Doesn't occur with rest).
Plaque buildup, high cholesterol, High blood pressure, smoking, diabetes. Chest pain that occurs at rest with no physical exertion or stress (S-T depression at time of attack; troponins not elevated)
|
Myocardial Infarction |
Persistent central chest pain (squeezing, pressure, or fullness). Pain may radiate to the shoulders, arms (usually left arm), neck, or back. Sweating, shortness of breath, dizziness, Nausea, and vomiting may also be present. Usually the patient might describe the pain as if an “elephant is sitting on his or her chest”. |
Blood clots, smoking, high blood pressure, obesity, diabetes, family history, lack of exercise, stress (S-T elevation, elevated troponins) |
Heart Valve Disease |
Tiredness and fatigue. Swelling of the feet, ankles and at times the abdomen. Shortness of breath with exertion or when lying down. Usually chest pain/discomfort with exertion. Dizziness or fainting. Heart palpitations. |
Rheumatic fever, infective endocarditis, Coronary Artery Diesease (CAD), Heart attack, or congenital abnormality. |
Arrhythmias |
Palpitations, pounding in your chest, dizziness, lightheadedness, weakness or fatigue, shortness of breath. |
Underlying heart disease, caffeine, tobacco, alcoholism, diet pills, and stress. |
Aneurysms (Aortic) |
Severe Ripping or tearing pain in the chest (ascending aorta), or pain between the scapulas (descending aorta). Difficultly breathing, coughing, hoarseness. |
Atherosclerosis, Hypertension, smoking, diabetes, Marfan's Syndrome, family history, hyperlipidemia, high blood pressure. |
Congestive Heart Failure
(frequently asked on the part IV) |
Breathlessness or shortness of breath(trouble breathing when lying down ), weight gain (retention of fluid in the body), fatigue. Swelling and fluid buildup in the ankles, feet and legs. Mental confusion and impaired thinking, Nausea and lack of appetite. Rapid and irregular heartbeat.
Patient may develop coughing due to fluid in the lungs. |
Coronary artery disease (CAD), weakened heart muscles, uncontrolled high blood pressure (left ventricular hypertrophy), smoking, obesity, diabetes, lack of physical activity, longstanding alcohol abuse. Heart valve problems/disorders.
|
Pericarditis |
Chest pain that is increased with reclining or lying down and improved with leaning forward. Low grade fever. Shortness of breath, fatigue, and feeling sick. Pain not related to physical activity. |
Idiopathic (most common), Viral Infection, Medications, AIDS, and Myocardial Infarction ( diffuse S-T elevation in all lealds) |
Back to Top of Page
Abdominal Examination:
It is important to review the 4 Quadrants of the abdomen and some of the important structures.
Memorize the structures listed below for each quadrant, for they are common causes of pain in those areas. You must ask specific questions to determine the true cause of the pain. Structures underlined are more common causes of pain in those quadrants.
Table 28.
RUQ
- Liver
- Gallbladder
- Pancreas
|
LUQ
- Stomach (epigastric region also)
- Spleen
|
RLQ
- Appendix
- Right ovary
- Right fallopian tube
|
LLQ
- Sigmoid colon
- Descending colon
- Left ovary
- Left fallopian tube
|
Epigastric pain
- Peptic ulcers
- Hiatus hernia/GERD
- Pancreatitis
- Gastritis
- Peritonitis
- Ruptured aortic aneurysm
|
|
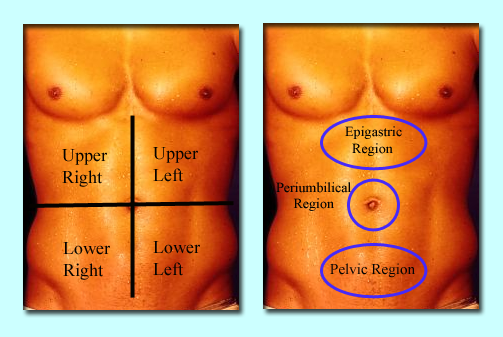 |
Back to Top of Page
Here are a few generalized questions that should be asked during the course of an abdominal examination to help you rule in or rule out a few conditions. Table 29 covers some of the more important areas that should be addressed while attempting to determine the true cause of the patient's problem.
Table 29.
Organ/Structure |
Question(s) |
Possible Diagnoses/Differential Diagnoses |
Hiatus |
- Do you experience heartburn or pain in the chest?
- Does lying down or bending forward cause the pain to worsen ?
- Do you feel bloated?
- Do you belch/burp constantly and have difficulty swallowing?
|
Hiatal Hernia |
Liver |
- Do you drink alcohol and if so how much?
- Any History of alcoholism?
- Any history of fatigue, sore throat, weakness, swollen cervical (neck) lymph glands?
- Do you have any joint pain, irregular heart beats, abnormal pigmentation or discoloration of the skin? Loss of sex drive? Fatigue? Abdominal Pain? Do any of your family members also have or have had similar problems?
|
Liver cancer, cirrhosis, enlarged liver or fatty liver.
(Unintentional weight loss could highly suggest Liver Cancer)
Hepatitis
Mononucleosis (enlarged liver)
Hemochromatosis
|
Gallbladder |
- Does your pain increase with certain foods like French fries/fast foods or fried or fatty foods ?
- Does your pain ever refer to the right shoulder posteriorly or do you have any associated symptoms such as right shoulder pain, nausea and vomiting?
|
Cholelithiasis (gallstones) |
Pancreas |
- Any radiating pain that shoots up the spine between the shoulder blades?
- Have you been drinking or have you had too much alcohol?
- Any fever, nausea or vomiting?
- Any relief if you lean forward or curl into a fetal tuck position?
|
Pancreatitis |
Spleen |
- Any trauma to your abdomen?
- Do you feel light headedness?
- Do you bleed more easily than usual?
- Feeling of fullness
- Pain in the upper left abdominal area(under the ribs)
- Any history of fatigue, sore throat, weakness, swollen cervical (neck) lymph glands?
|
Spleen rupture
Mononucleosis (enlarged spleen) --> an enlarged spleen can also rupture.
|
Stomach/GI
(can cause Left upper quadrant pain or epigastric pain) |
- Does your pain come shortly after a meal?
- Any pain during a meal?
- Any pain when you're hungry or have an empty stomach?
- Does your pain come a few hours(3-4) after eating a meal(when stomach becomes empty again)?
- Does your pain improve after you eat a meal?
- Does pain wake you up at nights or early morning ?
|
Gastric ulcer
Duodenal ulcer |
Appendix
(Pain usually starts in the middle of the abdomen around the umbilical area and moves down to the RLQ -->ask to see if the patient has experienced such symptoms) |
- Any nausea, vomiting, low grade fever, or loss of appetite?
|
Appendicitis
Note: If patient admits to having sudden relief of pain, this is an indication that the appendix has ruptured and patient should be referred out immediately or 911 should be called. |
Kidney
Most important differentiation between kidney stones and kidney infection would be the FEVER. |
- Any low back pain or flank pain?
- Any urinary frequency or pain during urination?
- Any blood in urine?
- Any nausea or vomiting?
- Is the pain cramping and spasmodic? (colicy)
- Does pain radiate into the groin or inner thigh areas?
- Any fever or chills?
- Any burning during urination?
- Any blood during urination?
- Fatigue
- Costo-vertebral angle tenderness
|
Kidney stones
Kidney infection (pyelonephritis)
|
Uterus |
- Any heavy or prolonged menstrual bleeding?
- Any pressure/heaviness in the lower abdomen?
- Frequent urination ?
- Any low back pain ?
|
Uterine fibroids |
Colon |
- Any abdominal pain? (mostly in left lower quadrant)
- Nausea or vomiting ?
- Blood in stools ?
- Fever or chills ?
- Constipation ?
- Cramping ?
- Unintentional weight loss ?
- Blood in stools?
- change in bowel habits such as diarrhea and constipation?
- a feeling of bowel not emptying completely?
- Stools are thinner than usual?
- Vomiting?
- Abdominal pain and bloating
|
Diverticulosis --> Diverticulitis
(common on the lower left quadrant = descending colon and sigmoid colon.)
Colon Cancer
|
Ovaries |
- Menstrual Irregularities?
- Pain in the lower abdomen or low back areas(even the hip)?
- Pain with intercourse?
- Infertility?
- Abdominal swelling?
- urinary frequency? (if cyst is large enough to put pressure on the bladder)
|
Ovarian cyst |
Fallopian Tube |
- Are you trying to get pregnant or are you sexually active ?
- Any low back pain or one sided lower abdominal pain ?
- dizziness or low blood pressure ?
- vaginal spotting or bleeding ?
- Tenderness in the breasts ?
- A missed period ?
- Any pain in the shoulder(s) ?
|
Ectopic pregnancy |
Abdominal Aorta |
- Do you have pulsatile sensation(s) near your umbilicus?
- Any abdominal pain or back pain?
- Any tearing or ripping like pain in your abdomen?
- Syncope?
|
Abdominal Aortic Aneurysm |
Prostate |
- Do you have difficulty starting or stopping urination?
- Do you have dribbling urination, urinary urgency and frequency?
- Do you frequently get up at nights to urinate?
- Do you have weak urination or do you feel that your bladder isn't empty after urination?
- Do you have painful urination?
|
Prostate related problems, (Benign hypertrophy, Prostatitis, Cancer)
Note: must find the underlying cause and differentiate which type of prostate problem the patient may have.
1. Benign Prostatic Hypertrophy
- weak stream
- dribbling urination
- urinary urgency and frequency
- possible low back pain
- NO fever
- NO weight loss
2. Prostatitis
- Fever and chills
- frequency and urgency (especially at nights)
- burning or painful urination
- possible low back pain
3. Prostate Cancer
- Unintentional weight loss (most important)
- All the things listed above for #1 and #2 but must have the patient admit to unintentional weight loss (this suggests cancer) and constipation
|
Cauda Equina |
- Do you have Urinary Incontinence or retention?
- Do you have bowel incontinence?
- Do you have sexual dysfunction?
|
Cauda Equina Syndrome |
Back to Top of Page
Inspection:
Look for any scars, masses, distension, striae (stretch marks), dilated veins, abnormal pulsations or peristalsis/movements, discolorations, rashes, vascular changes, hernias etc. Also make a note of the shape of the abdomen (scaphoid, flat, protuberant).
Auscultation:
Use the diaphragm of the stethoscope.
You may be asked to Auscultate the following structures/sounds:
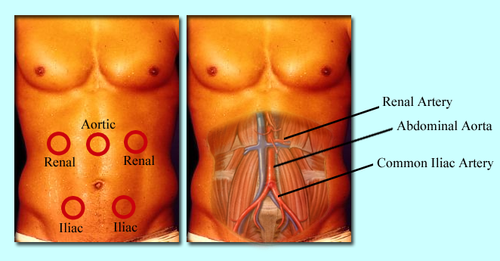
1. Bowel Sounds
|
2. Abdominal Aorta
|
3. Renal Arteries
|
4. Iliac Arteries
|
Table 30. Bowel Sounds
Hypoactive(decreased) |
Hyperactive(increased) |
Absent |
- Constipation
- Radiation therapy (chemotherapy)
- Low fiber diet
- Hypokalemia
- Hypercalcemia
- Peritonitis (can progress to absent bowel sounds)
|
- Crohn's disease
- Ulcerative colitis
- Diarrhea
- Early intestinal obstruction
|
- Bowel obstruction
- Peritonitis
- Paralytic Ileus
Note: To diagnose absent bowel sounds you must listen for 2 minutes. |
Back to Top of Page
Percussion:
Percussion is mostly used to determine the span and consistency of the liver, the spleen, or other underlying masses. It is also used to determine if abdominal distention is due to gas in the bowels, masses (tumors, pregnancy, fibroids etc.), or abnormal fluid in the abdominal cavity known as ascites.
Normally, tympany predominates in the abdomen with percussion but certain areas of dullness are also noted due to feces and fluid contained in the GI tract. Unusual dullness can be due to an underlying abdominal mass, an enlarged organ, or fluid accumulation in the abdominal cavity.
Table 31. Comparison of Tympany vs. Dullness during percussion of the abdomen
Tympany |
Dullnes |
- Most areas of the abdomen
- Intestinal gas
|
- Underlying mass or enlarged organ
- Feces and fluid in GI tract (normal)
- Fluid (ascites) --> perform shifting dullness
|
1. Percussion of the liver
- Percussion of the liver produces a dull sound (dullness).
- Used to detect the span of the liver/enlarged liver.
- If the patient informs you that he or she experienced pain during this examination, then there is a high chance that the patient might have a liver problem. (Again, you must ask questions to determine what kind of liver problem he or she may have. Refer to Table 29 above for possible liver related questions).
2. Percussion of the spleen
- Percussion of the spleen produces a dull sound (dullness).
- Used to detect the span of the spleen/enlarged spleen.
- Normally, it is very difficult to percuss the spleen. A change from tympany to dullness could suggest an enlarged spleen (splenomegaly). Area of dullness should be noted (this is called a “positive splenic percussion sign”)
Note: If the patient complains of pain during this examination, consider a problem related with the spleen. Refer to Table 29 above to determine what questions you would need to address (regarding the spleen) in order to determine the cause of the patient's complaint.
3. Shifting Dullness (Verbal Component)
- Used to confirm that the dullness produced with percussion of the abdomen while the patient was supine is due to fluid accumulation in the abdominal cavity.
- You will most likely be asked to perform this examination in the form of a verbal component. Here is an example of how it may be verbalized:
1. “Shifting dullness is used to detect fluid accumulation in the abdominal Cavity” (ascites) --> (shows that you know what the test is used for)
2. “Initially, I would percuss the patient in a supine position and note a shift from tympany to dullness, which could be a sign of ascites (fluid accumulation). To confirm that the dullness is due to fluid accumulation, I would then roll the patient away from me in a side lying position, and perform percussion again.”
3. Findings:
a) Positive finding(s) = the area of dullness will shift to the dependent site (the side the patient is lying on) due to fluid accumulation and tympany will shift/rise toward the top confirming ascites. Alternate way of saying it:
b) Positive finding(s) = If previous areas of dullness have shifted to areas where tympany was once present --> this confirms ascites.
Back to Top of Page
Palpation:
NBCE has in the past asked students to perform Light (Superficial) and Deep Palpation of the abdomen.
Table 32. Light (Superficial) vs. Deep Palpation of the abdomen.
Light (Superficial) Palpation |
Deep Palpation |
The examiner should push down about 1/2 inch with a light, gentle, dipping motion using the palmar surface of the fingers. Gentle rotating movements should be applied. Palpate the four quadrants in a clockwise direction, starting from the right lower quadrant. Make sure to palpate the painful area/region last. |
Examiner should push down about 2 to 3 inches using the palmar surface of the fingertips (use firm and steady pressure). The examiner may use both hands for this procedure with one hand on top of the other. Then, palpate the four quadrants in a clockwise direction, starting from the right lower quadrant. Make sure to palpate the painful area/region last. |
Used to assess superficial structures, including the subcutaneous tissue, and helps identify muscle resistance and tenderness. It also helps locate certain organs. |
Used to assess organs in the abdominal cavity. |
Note for any tenderness, masses or increased resistance. Normally, the abdomen is non-tender and soft. |
Note for tenderness, masses, pulsations, enlarged organs. |
Before you begin with palpation of the abdomen, instruct the patient to point to the area/region of pain. Again, remember to palpate the tender or painful region last. If the patient does not initially complain of pain, instruct the patient to inform you if any pain occurs as you begin palpating the abdomen. Also, look for any signs of apprehension as you perform this examination.
You will either be instructed to palpate a specific organ/structure (e.g. liver or abdominal aorta) or you may be instructed to perform either light/superficial or deep palpation of the abdomen as described above.
Palpation of the following structures may be asked:
1. Liver
- Normally, the edge of the liver is smooth and non-tender upon palpation.
Table 33.
Normal |
Metastatic Carcinoma |
Hepatitis |
Cirrhosis |
Smooth, non-tender with no irregularities. |
Very hard and nodular, enlarged and non-tender. |
Smooth, enlarged, tender. |
Smooth or nodular irregularity, large and non-tender.
|
Note: Other causes of tenderness in the liver can be due to congestion (heart failure) or, Mononucleosis (There are more causes of liver pain, however these are just a few important ones to consider).
2. Spleen
- The spleen is normally non-palpable.
- A palpable spleen indicates splenomegaly (enlarged spleen).
3. Abdominal Aorta
- Normal size of the abdominal aorta is about 2cm.
- Abdominal aortic aneurysm is considered when abdominal aorta reaches 3cm or greater.
4. Kidney
5. Note: It is also possible that you may be asked to palpate the entire abdomen (the four quadrants – light (superficial) and deep palpation. Be ready to differentiate the cause of pain in certain regions of the abdomen upon palpation. Refer to Table 28.
Also, when you complete the examination, ask the patient “Is there anything else you would like to tell me that I should know about or is there anything else that I haven't covered that may concern you?” (The patient may mention something important that was not covered by you.)
Back to Top of Page
Palpation of Pulses of Upper and Lower Extremities
- Radial Artery
- Brachial Artery
- Popliteal Artery
- Posterior Tibial Artery
- Dorsalis Pedis Artery
We recommend that you palpate the pulses bilaterally. Do NOT use the Thumb for this examination. Use the Index and Middle finger to assess the pulses. Note to see if the pulse is regular or irregular. Also note the rate, rhythm, amplitude, contour and symmetry of the pulses.
For assessment of the the Popliteal Artery, the patient should be supine with the knee in slight flexion. The examiner's hands should encricle the knee, pressing deeply into the popliteal space with the fingertips.
|
|
Case 2:
Below you will find another example of how a physical examination section may be presented and what is expected of you.
For example: 55 year old male complaining of abdominal pain.
Perform the following examinations: (Note: We have indicated the purpose of the examination and whether a test is normal, negative or positive; the actual NBCE examination will not display such findings, and will only display the names of the examinations that you will be required to perform).
1. Beevor's (indicative of spinal cord lesion)----negative
2. Rovsing's – (for appendicitis)----negative
3. Palpation of the liver---positive (patient complained of pain)
4. Murphy's punch---(kidney related problems)---negative
5. Auscultation of the abdomen --- Normal
|
Prior to beginning the examinations listed above, you must quickly take a mini 30 second history to determine what kind of a problem the patient is presenting with. In this case, you would definitely want the patient to point to the area of pain (abdominal pain can be vague and you would want to know specifically where the pain originates from and if there is any radiation of pain present.) Once you get the patient to specifically point to the area of pain, you should then quickly ask about how and when the pain started, if there was any trauma involved, any associated symptoms, type of pain (dull, sharp, achy, burning, deep, superficial etc) and if the pain is progressively getting worse? Some of these questions can direct you toward the right direction and quickly give you a few differentials to work with. Let us assume the patient stated that there was no trauma involved, his pain is progressively getting worse, the pain is difficult to describe and seems to be deep in nature over the right upper quadrant (RUQ). The patient seems to have minimal fatigue.
At this point, prior to starting the examinations listed above, you now know based on the mini history, that you are most likely dealing with either the Liver, Gallbladder or even the Pancreas. Now you must perform the examinations and ask specific questions to rule in or rule out one from the other.
After you have performed the examinations listed above and have asked the patient questions regarding each organ/structure displayed in (Table 29), the patient states that his symptoms are not worsened by eating certain fried or fatty foods (this rules out gallbladder disorder). Patient admits to being an alcoholic (so you're thinking possible liver or pancreatic problem). Patient denies any pain referred between the shoulder blades, having a fever at the moment or in the past, nausea, vomiting or any position that relieves the pain (rules out pancreatitis). Now you are leaning more towards the liver because palpation of the liver produced pain during the examination. At this point, it is now your objective to figure out what kind of a liver problem it might be (Cancer, Fatty Liver, Hepatitis, Cirrhosis, Obstruction, Mononucleosis or even possible Hemochromatosis). Therefore, you must now ask the patient about recent unintentional weight loss. If the patient admits to having unintentional weight loss, then Liver Cancer would be a good probable diagnosis (you must always look for associated symptoms that will help you prove the diagnosis of liver cancer such as unexplained fevers, frequently waking up at nights due to pain, pain that is hard to describe, muscle wasting, etc. Now, if the patient had stated that he has not experienced any unintentional weight loss, then it would be a reasonable indication that he has a liver problem but not necessarily liver cancer. At this point, you must take the patient's history under consideration and ask specific questions listed in (Table 29) to rule in or rule out all the other possible liver pathologies mentioned above. As you enter the post-station, you will also have additional information about the patient as well as x-rays and laboratory findings. Refer to the laboratory section while you are in the post-station to see if there are any changes in liver enzymes, which could also give you a clue to the type of liver pathology (refer to the clinical laboratory section of the review).
Now, after asking the patient specific questions, the patient admitted to being an alcoholic (has been drinking heavily for 2 years now), has been experiencing minimal fatigue, no unintentional weight loss, no change in weight; no fever at the time of examination or in the past, no swollen glands, no pigmentation on the skin and no joint pain. Rovsing's, Murphy's punch, Beevor's were all negative as shown above, and auscultation of the abdomen was normal. Palpation of the liver produced pain. X-ray findings are normal. Blood tests reveal an increase in liver enzymes, cholesterol, and triglycerides. No elevation in WBCs observed; Iron and Ferritin levels are within normal levels. In the post station, you see the following options.
A) Choose one symptom and two diagnoses.
1. Liver Cancer
2. Right Upper Quadrant pain *
3. Mononucleosis
4. Hepatitis
5. Hypercholesterolemia*
6. Gallstones
7. Right lower quadrant pain.
8. Kidney infection
9. Alcoholic induced fatty liver *
10. Pancreatitis |
B) Choose three appropriate management options for this patient.
1. Pancreatic biopsy
2. Refer the patient out to a medical doctor and follow up *
3. Referral to an Orthopedist for joint pain
4. Advise patient to completely stop consuming alcohol*
5. Immediately call 911
6. Liver biopsy
7. Order a genetic test for hereditary hemochromatosis
8. Liver Ultrasound*
9. Over the counter medication for abdominal pain
10. Monospot Test |
Lets review the answers in Section A and Section B.
Section A interpretation:
1. If you did not ask the patient to locate the area of pain during the mini-case history or during the time of the examination, then you would have never known that the patient presents with RUQ pain because the initial history stated that patient presents with abdominal pain (non specific area).
2. Laboratory tests confirmed that the patient has hypercholesterolemia (if you did not look in this section, you would have missed this answer.)
3. Alcohol induced fatty liver is also one of the answers because it was confirmed during the history taking that the patient has been consuming alcohol heavily for 2 years and the laboratory findings in the post station confirmed changes in the liver markers. Certain conditions were ruled out because the patient did not present with certain symptoms associated with these conditions such as:
- No fever, and WBC's were within normal limits in the laboratory section– helped rule out Hepatitis.
- No sore throat, no enlarged lymph nodes, and no severe fatigue – helped rule out Mononucleosis.
- Iron and Ferritin levels were within normal levels and patient had no joint pain or abnormal discoloration of the skin – helped rule out hemochromatosis.
- No unintentional weight loss, no waking up at nights due to pain – helped rule out Liver Cancer.
- Pain was not caused by or made worse with consumption of fried or fatty foods – helped rule out gallbladder disorder.
- Patient denies any pain referred between the shoulder blades, having a fever at the moment or in the past, nausea, vomiting or any position that relieves the pain -- helped rule out Pancreatitis.
- Rovsing's Test was negative – Also helped rule out possible Appendicitis.
|
Note: Although the objective findings, subjective complaints, and laboratory findings indicate fatty liver as a diagnosis, diagnostic testing such as Ultrasound, MRI, CT or Liver Biopsy should be performed to confirm this diagnosis.
Section B interpretation:
1. It is important to note that when a patient presents with a true "medical condition" that it be managed by a medical doctor. This referral is medically appropriate and necessary as well as essential for proper patient management.
2. With an alcohol induced fatty liver, it is important that the patient eliminates all alcohol consumption immediately to ensure proper recovery.
3. Although Liver biopsy would also be an appropriate answer, it is more invasive for this type of condition. Therefore, Ultrasound is more appropriate for diagnosing fatty liver. Note: If you notice that more than one answer may be correct, always choose an answer that is less invasive as described above.
This example allowed you to see how essential it is to take a through history as you perform the examinations. The post station questions are composed of a series of answers, which are directly linked to the actual diagnosis as shown above. Therefore, the examination findings, x-rays, and clinical laboratory findings are mainly used to assist you in determining the final diagnosis and the answers in the post-stations.
As a general rule, if an examination produces pain such as the case with liver palpation, it is highly probable that the patient will have a liver problem. For example: NBCE will not have a patient admit that he or she has pain with Murphy's punch (used to diagnose kidney related problems) and have the diagnosis be related to the heart. The examinations that you perform will help you determine the site of pathology or problem, but it would be your objective to find the true cause of the problem by asking specific questions before and after you perform the examinations as shown in the example above.
Once again, detailed questions must be asked in order to properly diagnose the patient. You are given points for correctly performing examinations, asking appropriate types of questions, and for your professionalism/patient consideration.
Back to Top of Page
Conclusion:
-
Have a few differentials as you enter the room.
-
You may use a sanitizer if available (although you don't have to).
-
Introduce yourself to the patient prior to beginning your examination.
-
Ask a few questions prior to starting the examination such as how it happened, when it happened, if there was any trauma involved, any associated symptoms (a quick mini 30 second history prior to beginning the examination will give you an idea of what you're dealing with).
-
Relax and don't be nervous; The examination is indeed straightforward, easy and fun.
-
Remember that the patients are acting out conditions and will respond or give you valuable information based on the types of questions you ask them. (so make use of the questions we have provided for you in this section and the Case History Section).
-
You will not be able to talk to the doctor(s) observing you. They are simply there to assess your performance.
-
Before you perform an examination that is listed on the paper (in the hallway and inside the room), make sure you DO NOT miss the Verbal Components --> this would be the only time that you speak to the observing doctor. Remember you must perform the examination on the patient and describe your findings to the doctor.
-
Make sure you are using the appropriate instrument for the examination.
-
If you're done before the time has elapsed, DO NOT sit and wait (this could cost you points). Continue asking questions or expand on areas that may concern you.
-
Most importantly, we advise that you DO NOT constantly read or ask questions directly from your notes (cheat-sheet) when you're with the patient, you must be ready for this examination. You will be given a scratch paper to write down notes or reminders but do not rely on the notes to help you get through the examinations. Using your notes/cheat-sheets consistently may not leave a good impression and it may make it seem like you were not prepared for this examination. We advise that you use this paper to write down your findings or other valuable information that may come up during the examination.
-
Remember, you will only have 5 minutes to fully perform your examinations and ask all the necessary questions.
|
Back to Top of Page
Good Luck and Thank You for Choosing CNBA
|